Adult vaccinations
Last Modified 16/10/2025 08:34:02
Share this page
Introduction
The UK has a comprehensive routine vaccination schedule that aims to provide protection against a wide range of vaccine preventable infectious disease and their complications.
The majority of these vaccinations are offered in childhood and information on childhood immunisations can be found at Childhood immunisations (0-4 years) and Childhood immunisations (5 years and over).
Vaccination eligibility for the adult population is based on risk factors with the most common ones being age, pregnancy and a wide variety of medical conditions and social factors. The full routine schedule can be found here:
Figure 1: Summary of the age based routine adult vaccinations
| | Vaccination | Frequency |
|---|
| Age 65 |
Pneumococcal |
Once |
| Age 65 and over |
Influenza |
Annually |
| Age 65-79 (recent change) |
Shingles |
Once |
| Age 75 |
Respiratory syncytial virus (RSV) |
Once |
| Age 75 and over (recent change) |
COVID-19 |
Annually |
| Source: UK Health Security Agency (UKHSA), Complete routine immunisation schedule from 1 September 2025 |
This report will focus on vaccinations with the widest eligibility and the most available data sets. This includes all age-based vaccinations, at risk groups and healthcare workers for influenza vaccinations and pregnant women for pertussis vaccination.
Facts, figures and trends
-
- Influenza vaccination uptake in Blackpool for 2023/24 was 74% for over 65s and 38.5% for at risk groups. Both lower than the England average and falling from the previous year.
- Pneumococcal vaccination coverage in Blackpool for 2022/23 for over 65s was 70.7%.
- Prenatal pertussis vaccination coverage in Blackpool for 2025 is 60.8%, representing the second year on year rise yet remaining below the England average.
- Shingles vaccination coverage for adults in Blackpool turning 71 in 2022/23 was 41%, also representing a second year on year rise but remaining below the England average.
Influenza vaccination
The Influenza (flu) vaccination is offered annually to all adults over the age of 65, all frontline healthcare workers, pregnant women and people at increased risk of flu complications due to a wide range of medical conditions.
Figure 2: Trend in flu vaccination uptake for adults over 65 over the last 5 completed flu vaccination seasons
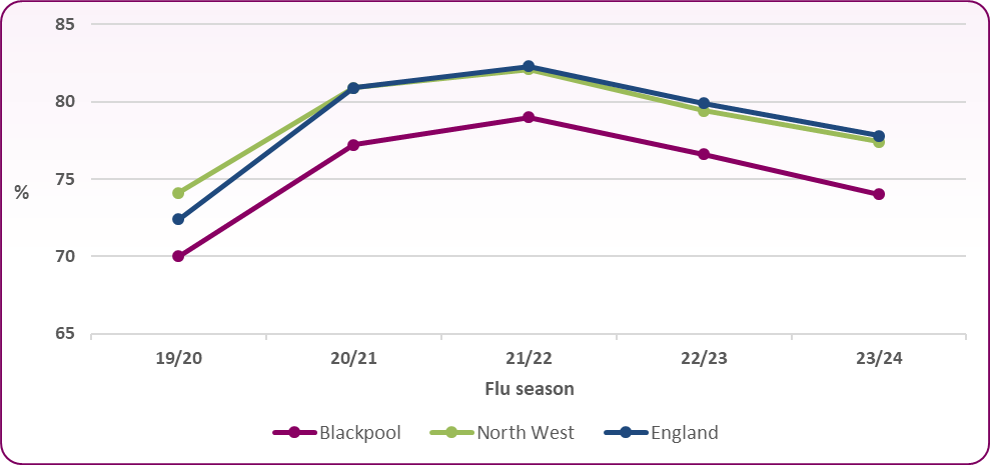 Source: UKHSA, Seasonal flu vaccination uptake figures1
Source: UKHSA, Seasonal flu vaccination uptake figures1
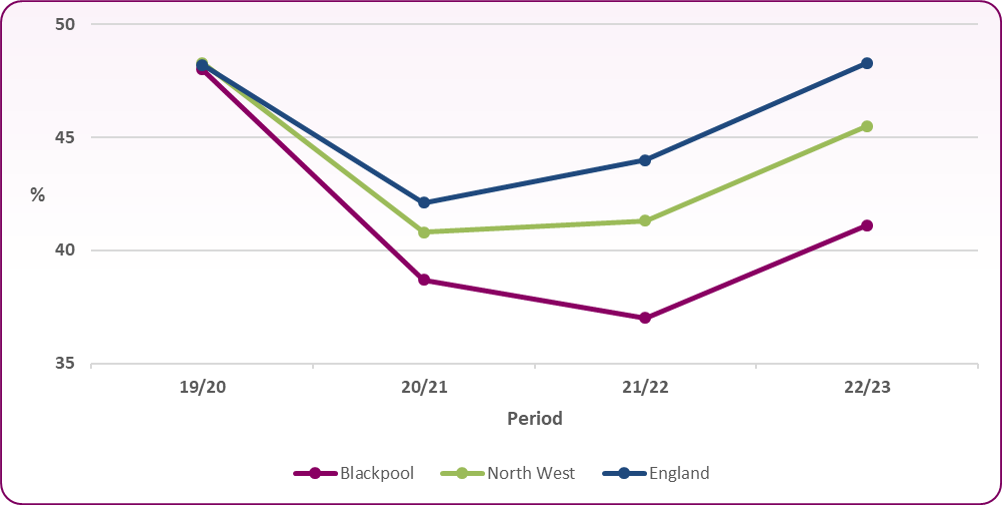
Figure 3: Trend in flu vaccination uptake for at risk individuals over the last 5 completed flu vaccination seasons*
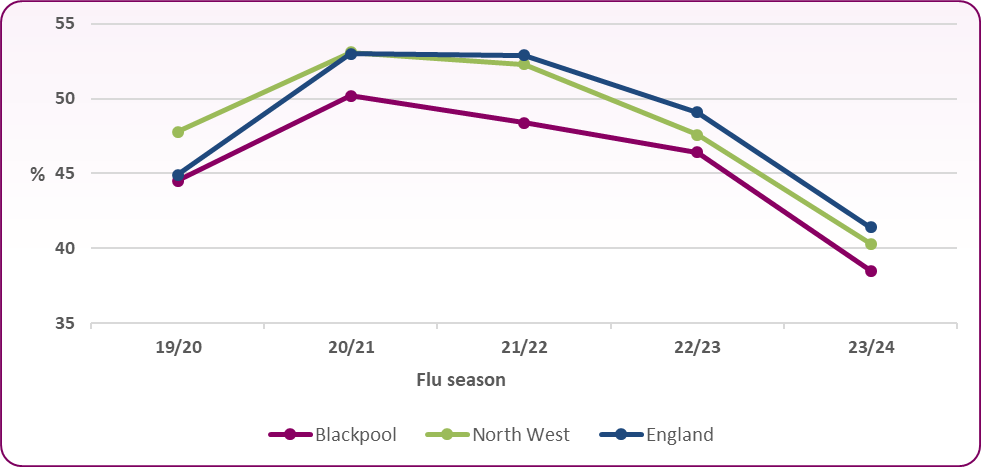 Source: UKHSA, Seasonal flu vaccination uptake figures1
Source: UKHSA, Seasonal flu vaccination uptake figures1
*Note the population group covered by this data set includes all individuals aged 6 months to 65 years excluding pregnant women - in one or more clinical risk groups.
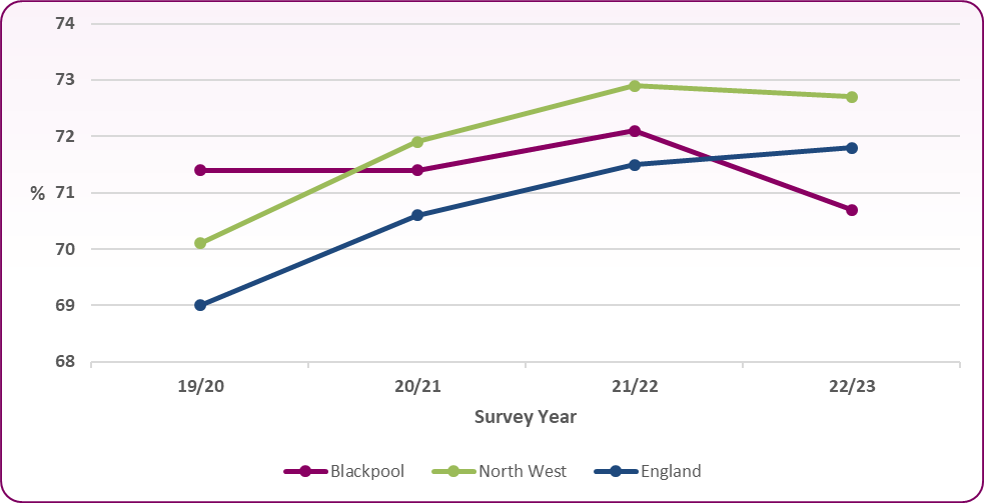
The World Health Organisation (WHO) target for seasonal flu vaccination for over 65s and at risk groups is 75% coverage and this is the target in use by UKHSA2. The above data shows that the most recent flu vaccination coverage in Blackpool for both groups is below the target level. Coverage is significantly higher for over 65s (than at risk groups) and only fell below the 75% target in the 2023/24 flu season.
In both groups, the coverage trends for Blackpool broadly follow those of both England and the North West with rising coverage from 2019/20 to 2020/21 season followed by a stagnation and decline in coverage in following years to 23/24. In both groups, despite following the regional and national trends, the actual percentage coverage for Blackpool remains around 3% lower than national average over all the included seasons.
Figure 4: Percentage flu vaccination coverage among all frontline staff at Blackpool Teaching Hospitals compared to England average for the last 2 flu seasons
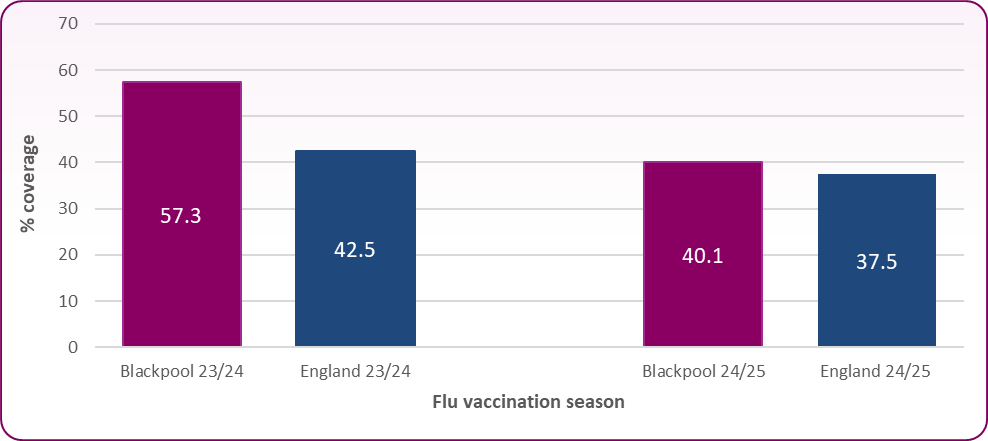 Source: UKHSA, Seasonal influenza vaccine uptake in frontline healthcare workers in England: winter season 2024 to 2025 data
Source: UKHSA, Seasonal influenza vaccine uptake in frontline healthcare workers in England: winter season 2024 to 2025 data
Figure 5: Percentage flu vaccination coverage by staff group for frontline healthcare workers at Blackpool Teaching Hospitals
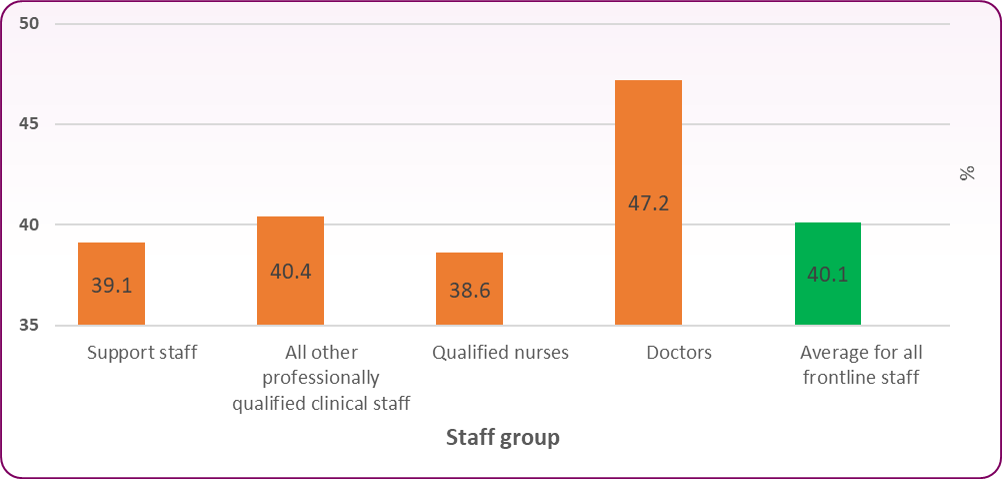 Source: UKHSA, Seasonal influenza vaccine uptake in frontline healthcare workers in England: winter season 2024 to 2025 data
Source: UKHSA, Seasonal influenza vaccine uptake in frontline healthcare workers in England: winter season 2024 to 2025 data
The data shows that flu vaccination coverage among frontline healthcare workers is higher at Blackpool Teaching Hospitals than the England average however both the level of coverage and the gap between Blackpool and England decreased from the 2023/24 season to the 2024/25 season. Once the data is broken down by staff group for Blackpool Teaching Hospitals, it shows the lowest coverage levels among qualified nurses and support staff, however coverage is less than 50% across all staff groups.
Respiratory syncytial virus (RSV) vaccination
Figure 6: RSV vaccination coverage rates for Blackpool and England, alongside refusal rate for Blackpool for adults turning 76-79 in 2024/25*
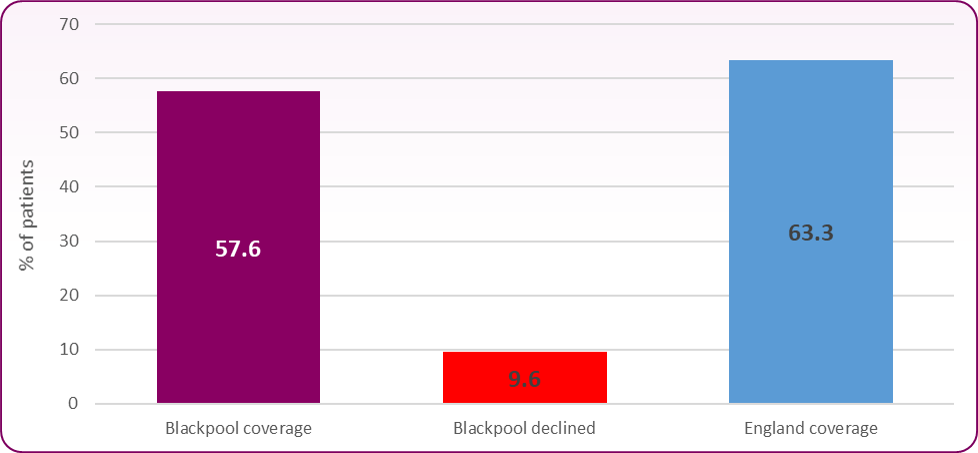 Sources:-
Sources:-
*Note there is a slight variation in the end point of the data collection with the Blackpool data ending 23/7/25 and the England data ending 31/7/25 (a difference of 8 days). Both data sets include patients with DOB 01/09/1945 to 31/08/1949. The patients turning 75 are not included in this data set as the year is not complete and not all have become eligible for the vaccination.
The RSV vaccination programme began in September 20243 and therefore the data lacks a time-based trend in uptake. The GP organisation level data for Blackpool did show the percentage of patients who declined the offer of vaccination which is reasonably low at just under 10%. This suggests that most of the patients not yet covered by the vaccination programme have potentially not been offered the vaccination, perhaps due to lack of regular contact with their GP practice. The data shows coverage level for Blackpool is 5.7% lower than the England average, and there is no North West level data for comparison.
COVID seasonal booster vaccination
Eligibility for the COVID seasonal booster vaccination currently includes all adults over 75, anyone living in a care home for older adults and anyone aged 6 months to 75 with a weakened immune system4. The age based eligibility was changed from over 65 to over 75 after the autumn 2024 vaccination period5. There is GP organisation level vaccination coverage data available for Blackpool and there is coverage data for England however there are no reasonably comparable cohorts between these data sets. In Blackpool, COVID vaccination rates for over 65s in the spring 2025 period were 27.6%6 (note - 1 of 17 GP organisations did not respond to the survey and by this period only over 75s were eligible based on age alone). For England, average spring 2025 COVID vaccination uptake for over 75s is 60.3%7 however these figures are not directly comparable due to the different age groups and the figures do not include the patients vaccinated in the autumn 2024 period.
Pneumococcal vaccination
Figure 7: Trend in pneumococcal vaccination coverage for over 65s
 Source: UKHSA, Population vaccination coverage: PPV1
Source: UKHSA, Population vaccination coverage: PPV1
Unlike the data for seasonal flu vaccination uptake, this data shows no sustained downward trend in pneumococcal vaccination coverage locally, regionally or nationally. However this data only extends to the 2022/23 season and not 2023/24 so it will be useful to see further trends when the next season’s data is released. In the 2019/20 season, pneumococcal vaccination coverage rates in Blackpool were higher than regional and national rates however this is no longer the case by 2022/23.
Mortality from respiratory diseases
Figure 8: Respiratory disease mortality per 100,000 people per year
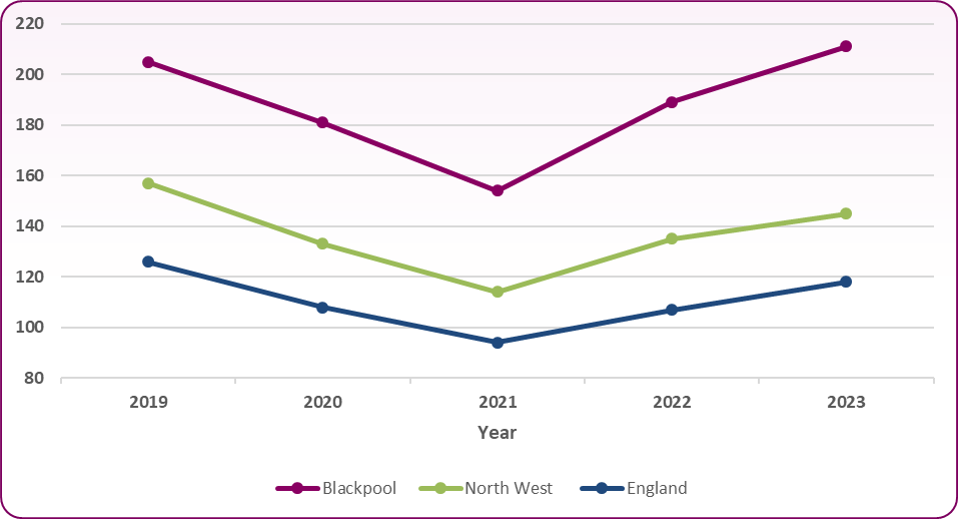 Source: DHSC, Mortality from respiratory diseases [1]
Source: DHSC, Mortality from respiratory diseases [1]
The above chart shows the trends in the rate of deaths where the underlying cause is recorded as any respiratory disease (ICD codes J00 to J99) for people of all ages. It is important to note that by no means are all deaths from respiratory diseases preventable by vaccination or even caused by infectious diseases. At a more disease specific level, the mortality rate (per 100,000 people) from influenza and pneumonia for 2021-23 for Blackpool is 66.2, compared to 43.8 for the North West and 34.2 for England. Similarly for the COVID mortality rate over the same period, Blackpool experienced 70.2 deaths per 100,000 compared to 60.5 for the North West and 57.5 for England1.
It is also important to highlight that there are a wide range of variables alongside vaccination that can affect respiratory disease mortality, and no statistical analysis has been carried out to attempt to draw any correlation between vaccination rates and respiratory disease mortality. This data has only been included to highlight that Blackpool has a higher rate of mortality from respiratory diseases than regionally or nationally and that this rate has risen for two consecutive periods. This higher rate suggests that Blackpool residents would likely benefit from any evidence-based interventions to reduce respiratory mortality, and it is likely that improving vaccination uptake/coverage rates for respiratory infections may be part of that.
Prenatal pertussis vaccination
Figure 9: Prenatal pertussis vaccination coverage*
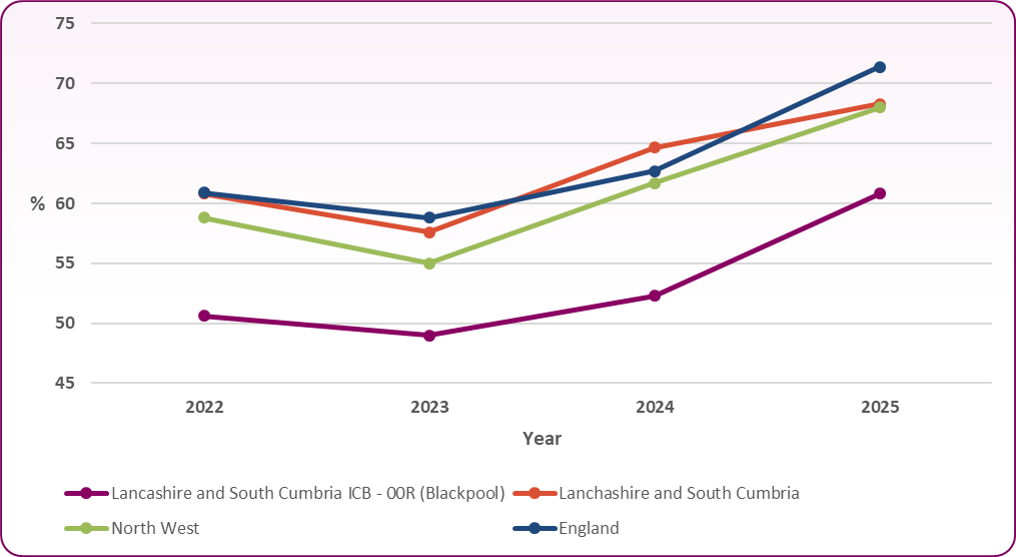 Source: UKHSA, Prenatal pertussis coverage estimates by local team, NHS commissioning region and integrated care board: England, January to March 2025
Source: UKHSA, Prenatal pertussis coverage estimates by local team, NHS commissioning region and integrated care board: England, January to March 2025
*Note monthly data was available from July 2022 to March 2025 and mean value was calculated for each year, meaning for 2022 and 2025 the mean value is not derived from a complete year’s worth of monthly data. This data is also based on NHS regions unlike much of the previous data, meaning the whole Lancashire and South Cumbria ICB can also be included for comparison.
For prenatal pertussis vaccination coverage, Blackpool has a lower percentage coverage than the three other regional to national comparators. At all geographical levels including Blackpool, there has been a two-year trend of increasing coverage rates.
Shingles vaccination
Figure 10: Percentage shingles vaccination coverage for adults turning 71
 Source: UKHSA, Shingles vaccination coverage (71 years) [1]
Source: UKHSA, Shingles vaccination coverage (71 years) [1]
This data shows the coverage rate of the shingles vaccination for adults turning 71 between 1 April and 31 March, and were vaccinated by the end of June1 for each period. There is a fall in coverage locally, regionally and nationally from 2019/20 followed by an improvement for all shown geographies from 2021/22 to 2022/23. However, coverage rates in Blackpool have fallen below those of the North West and England.
Summary of findings and trends
The trend over approximately the last 5 years shows vaccination coverage/uptake indicators for Blackpool remain inferior to regional and national averages for most of the key adult vaccinations. The main exception to this is the uptake of seasonal flu vaccination for healthcare workers at Blackpool Teaching Hospitals which is higher than national average. The time-based trends show seasonal flu vaccination uptake for those at risk based on age or medical conditions has declined over the past 2 years in Blackpool while prenatal pertussis vaccination and age-based shingles vaccination coverage has improved over a similar time period. Comparing average uptake/coverage rates across the whole included time frame shows seasonal flu vaccination uptake is much higher in adults eligible due to age than those eligible due to medical conditions and that pneumococcal vaccination coverage is much higher than shingles.
Challenges in increasing adult vaccination uptake/coverage
Factors that prevent more people from receiving the vaccinations that they’re eligible for the in the UK are broad but generally fall into two main categories: practical challenges or patient preference. The practical challenges include patients not being able to easily access or receive vaccination invitations, information or convenient clinic locations or times. Examples of patient preference challenges include phobias like needles or side effects, lack of trust in healthcare institutions or trust in safety and efficacy of vaccinations8. There are also specific population groups which are more likely to be affected by these factors and therefore have lower vaccination uptake.
Further information about key barriers to vaccination and specific populations groups from NICE are available at Vaccine uptake in the general population
The Vaccine Confidence Project is a research group founded in 2010 and partnered with multiple trusted international educational organisations and the WHO. It’s large-scale international surveys have found that vaccine confidence in the UK is high compared to other countries. However vaccination confidence indicators for the UK fell slightly between surveys conducted in 2015 and 2020. The demographic trends in vaccine confidence indicators are also notable as they generally show reduced vaccine confidence in younger age cohorts9. Further information from the Vaccine Confidence project about the UK can be found here: Vaccine Confidence Project - UK
Local and national strategies and guidance
-
- A Vaccine Bus service has been commissioned to deliver seasonal COVID and flu vaccinations on a walk-in basis at different locations within Blackpool to improve convenience of access.
- The Care Home Vaccination Pilot, as part of the Test to Change scheme involved a trial of a scheme for registered nurses employed at nursing homes to be trained and equipped to deliver vaccinations to both staff and residents within their facility. The scheme ran from November 2024 to January 2025 and was funded by the ICB. There was also the added advantage of helping to vaccinate bank staff and therefore the protection from vaccination was extended to other care facilities that these staff would work in.
- Bug Buster sessions are a new educational service started in 2024 that involves health protection nurses from Blackpool Council delivering teaching to adult social care staff on a range of infection prevention and control (IPC) topics including vaccination.
- In response to feedback from adult social care providers, the IPC Care Home Forum has been created to provide a setting for more regular information sharing on a range of topics (including vaccination) between the health protection team at Blackpool Council and care providers. It also facilitates care providers sharing learning and experiences with each other.
- Updated national information about vaccination is available from ‘The Green Book’
- National guidance more specific to vaccination uptake is available from the NICE guideline ‘Vaccine uptake in the general population’
[] Office for Health Improvement and Disparities. Public health profiles, 2025, https://fingertips.phe.org.uk/ , © Crown copyright 2025, accessed 11/09/2025
[] UKHSA, Seasonal influenza vaccine uptake in GP patients in England: winter season 2024 to 2025
[] UKHSA, RSV vaccine coverage report in older adults for catch-up cohorts in England: July 2025
[] NHS – COVID-19 Vaccine, https://www.nhs.uk/vaccinations/covid-19-vaccine/, (accessed 11/09/2025)
[] NHS England - Flu and COVID-19 Seasonal Vaccination Programme: autumn/winter 2024/25 (accessed 23/09/2025)
[] Immform, GP practice level COVID vaccination data for Blackpool (generated 09/09/2025)
[] NHS England, Spring 2025 Monthly COVID vaccinations 26 June 2025
[] NICE, Vaccine uptake in the general population, 2022
[] Vaccine Confidence Project, https://www.vaccineconfidence.org/vci/country/gb/, (accessed 15/09/2025)