HIV and AIDS
Last Modified 22/03/2023 12:03:28
Share this page
Introduction
Public Health England (PHE) report an estimated 105,200 people were living with HIV in 2019. The overall prevalence in the UK in 2019 was 2.4 per 1,000 people aged 15 to 59 years of age. Based on 2019 data, an estimated 94% of people living with HIV in the UK are diagnosed, 98% of those diagnosed are on treatment and 97% of those are virally suppressed. Overall, 89% of people living with HIV in 2019 had an undetectable viral load and were unable to pass on their infection1.
Free and effective antiretroviral therapy (ART) in the UK has transformed HIV from a fatal infection into a chronic but manageable condition. People living with HIV in the UK can now expect to have a near normal life expectancy if diagnosed promptly and they adhere to treatment. The population groups who have been most at risk of HIV in the UK have been GBMSM and black African people. With progressive strengthening of combination prevention (including condom use, expanded HIV testing, prompt antiretroviral therapy and availability of pre-exposure prophylaxis), HIV transmission, AIDS and HIV-related deaths could be eliminated in the UK.
People at risk of HIV can also use HIV pre-exposure prophylaxis (PrEP) to reduce the risk of establishing a permanent infection if exposed to the virus during sex.
The geographical distribution of people seen for HIV care and treatment is not uniform across or within regions in England. Knowledge of local diagnosed HIV prevalence and identification of local risk groups can be used to help direct resources for HIV prevention and treatment.
The Blackpool Sexual Health Needs Assessment 2021 presents a picture of all sexual health needs and service provision for sexual health in Blackpool and supports the development of the Sexual Health Strategy and Action Plan for Blackpool. The information on HIV and AIDS in Blackpool should be read in conjunction with this wider Sexual Health Needs Assessment.
Prevalence
In 2019 there were 381 Blackpool residents aged 15-59 seen at HIV services. Among those living with diagnosed HIV in Blackpool, 94% were white, 2% black African and 4% of 'other' ethnic origin. With regards to exposure, 77% most likely acquired their infection through sex between men and 18% through sex between men and women.
The diagnosed HIV prevalence rate was 4.9 per 1,000 population aged 15-59 years, compared to 2.4 per 1,000 in England (figure 1) . This has increased from the 2013 rate of 3.4 per 1,000 population. Blackpool is the only authority in Lancashire above the threshold whereby testing is recommended in general settings including all medical admissions and all new registrations in general practice (ie, 2 per 1,000 or 200 per 100,000).
Figure 1: HIV diagnosed prevalence rate, 2011-2019
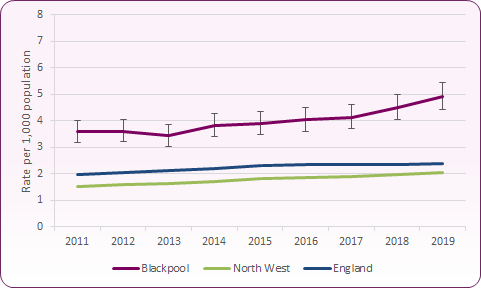 Source: PHE, Sexual and Reproductive Health Profiles
Source: PHE, Sexual and Reproductive Health Profiles
Figure 2 shows that Blackpool has one of the highest diagnosed HIV prevalence rates in the North West, and is one of nine local authority districts with a diagnosed HIV prevalence rate in excess of 2 per 1,000 population, the threshold for expanded HIV testing. A further increase in diagnosed prevalence will result in Blackpool being considered an 'extremely high prevalence' area alongside Manchester (6.2) and Salford (5.2).
Figure 2: Diagnosed HIV prevalence per 1,000 residents aged 15-59 years by district in the North West, 2019
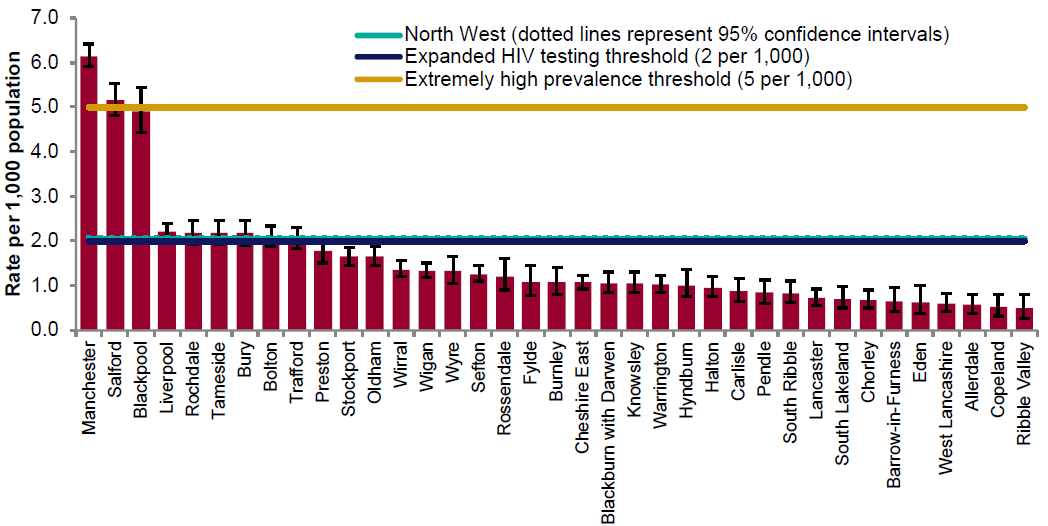 Source: PHE, HIV and Aids Reporting System (HARS); ONS population estimates 20197
Source: PHE, HIV and Aids Reporting System (HARS); ONS population estimates 20197
New HIV diagnoses
New HIV diagnosis is not synonymous with prevalence; however, it provides a timely insight into the onward HIV transmission in a country and consequently allows targeting efforts to reduce transmission. Although the majority of HIV diagnoses are made in genitourinary medicine (GUM) services, HIV testing has been introduced in a variety of different medical services and non-medical settings, including the expansion of self-sampling/self-testing2.
In the North West, 391 residents were newly diagnosed with HIV in 2019, a reduction of 21% from 20183. 47% of new diagnoses in 2019 were in men who have sex with men, a 35% reduction from 2018. 21% of new diagnoses in the region were among Black Africans. The number of new diagnoses was highest in the 35-49 year age group.
In Blackpool, the new diagnosis rate for residents aged 15 years or older in 2019 was 12.2 per 100,000, above that of both the North West (6.5) and England (8.1 per 100,000) (figure 3).
Figure 3: New HIV diagnosis rate per 100,000 people aged 15+, Blackpool, North West and England
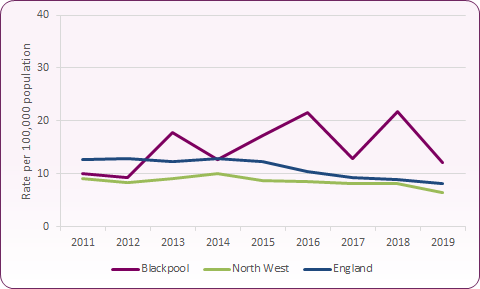 Source: PHE, Sexual and Reproductive Health Profiles
Source: PHE, Sexual and Reproductive Health Profiles
Blackpool's new diagnosis rate of 12.2 is the third highest among local authorities in the North West, behind Manchester and Salford (figure 4).
Figure 4: New HIV diagnosis per 100,000 population aged 15+ by NW local authority, 2019
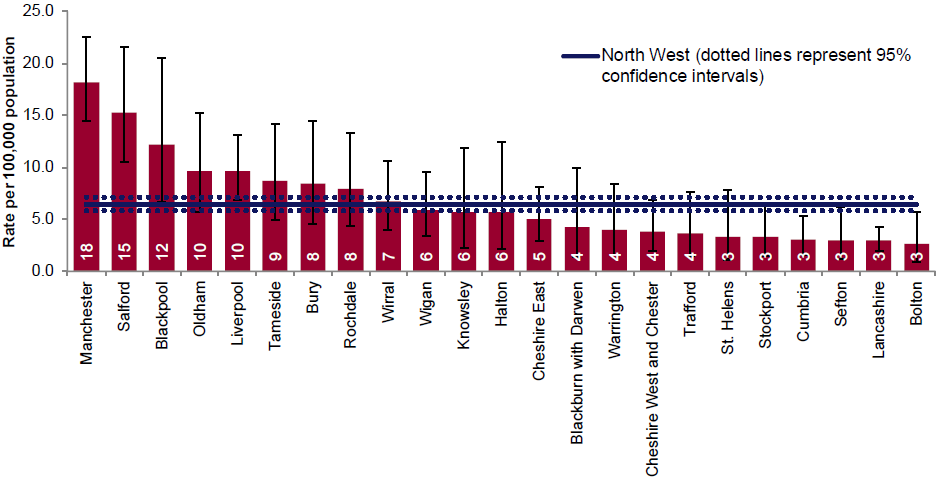 Source: PHE, HIV and Aids New Diagnosis Database (HANDD); ONS population estimates 20193
Source: PHE, HIV and Aids New Diagnosis Database (HANDD); ONS population estimates 20193
HIV testing and uptake
HIV test coverage data represent the number of persons tested for HIV and not the number of tests reported. HIV testing is integral to the treatment and management of HIV. Knowledge of HIV status increases survival rates, improves quality of life and reduces the risk of HIV transmission. As figure 5 shows, the percentage of eligible new GUM patients who accepted a test, as a proportion of those eligible, is higher than the England average total.
Figure 5: HIV testing coverage (%): 2019
| | Total | Men | Women | MSM |
|---|
| England |
64.9 |
78.3 |
55.8 |
87.2 |
| North West |
56.5 |
75.0 |
45.5 |
87.8 |
| Blackpool |
70.8 |
79.3 |
55.8 |
87.2 |
| Source: PHE, Sexual and Reproductive Health Profiles |
Figure 6 shows that HIV testing coverage in Blackpool has been consistently higher than the North West average since 2009 and, with the exception of 2016, higher than the England average since 2013.
Figure 6: Trend in HIV testing coverage in Blackpool, 2009-2019
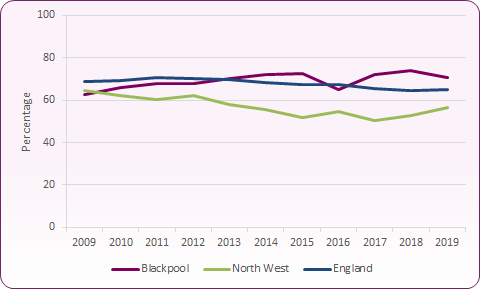 Source: PHE, Sexual and Reproductive Health Profiles
Source: PHE, Sexual and Reproductive Health Profiles
Routes of HIV infection
Of the estimated 105,200 people living with HIV in the UK in 2019, 48% are thought to be gay or bisexual men. Figure 7 shows that across Blackpool infection from sex between men remains by far the highest exposure route (77% in 2019). Whilst the number of people living with HIV in Blackpool increased across most exposure groups between 2015 and 2019, the proportion of those whose probable route of HIV infection was sex between men reduced from 81% to 77%.
Nationally and regionally, there has been a decline in HIV diagnoses where the probable exposure was through sex between men. The decline in new HIV diagnoses among gay and bisexual men (particularly those of white ethnicity) is a reflection of a combination of HIV prevention approaches in the UK including condom provision, pre-exposure prophylaxis (PrEP), expanded HIV testing and prompt initiation of treatment. Whilst predominantly focussed on London, these declines are beginning to be observed elsewhere.
Nationally, new diagnoses among people who probably acquired HIV through heterosexual contact also declined in 2019. In 2019 in the North West sex between men and women narrowly became the most common reported route of infection. This appears to be due to a sharp decline in new diagnoses among MSM, whilst cases of heterosexual transmission have remained relatively stable since 2015.
The transmission of HIV through injecting drug use is low and accounted for around 1% of the diagnosed HIV population Blackpool and across the North West in 20191.
Figure 7: HIV Exposure Groups, Blackpool and England comparison, 2019
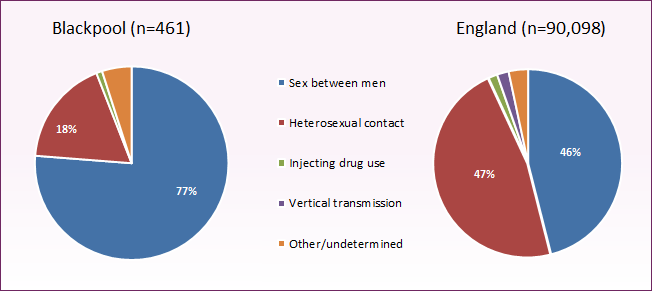 Source: PHE, HIV and STI Portal
Source: PHE, HIV and STI Portal
Late diagnoses
In the UK, many people are diagnosed at a late stage of HIV infection - this is defined as having a CD4 count under 350 within three months of a diagnosis. People living with HIV can expect a near-normal life span if they are diagnosed promptly. People diagnosed with HIV late continue to have a ten-fold increased risk of death in the year following diagnosis compared to those diagnosed early1.
Key strategic priorities for HIV are to reduce the proportion of late HIV diagnoses and to increase the proportion of HIV infections diagnosed. Late diagnosis is the most important predictor of morbidity and mortality among those with HIV infection and it is essential to evaluate the success of expanded HIV testing. This indicator directly measures late diagnoses; over time it will show whether there is a trend towards earlier diagnosis.
In Blackpool between 2017 and 2019, 26.5% of HIV diagnoses were made at a late stage of infection (CD4 count <350 cells/mm³ within 3 months of diagnosis) compared to 43.1% in England (figure 8). 25.7% of HIV diagnoses among MSM in Blackpool (34.1% nationally) and 33.3% of diagnoses of heterosexual women were at a late stage of infection. Nationally and regionally, late diagnosis was more common among new HIV diagnoses in heterosexual males (58.0% of diagnoses in England and the North West) and heterosexual females (48.6% in England and 46% in the North West). Data relating to heterosexual men in Blackpool for this period was suppressed due to low numbers.
Figure 8: % HIV late diagnosis Blackpool, North West and England, 2009-11 to 2017-19
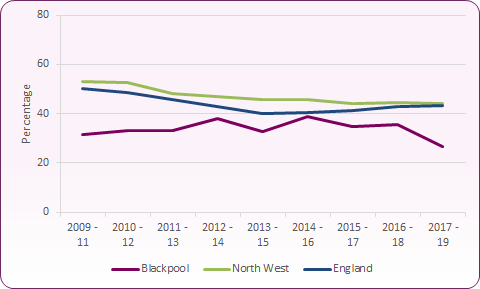 Source: PHE, Sexual and Reproductive Health Profiles
Source: PHE, Sexual and Reproductive Health Profiles
The high prevalence and continuing new incidence of HIV in Blackpool suggests a need to ensure the maintenance of services to support people who are living with HIV. However, the higher rates of new infections amongst men who have sex with men in Blackpool suggest there is a need for continuing targeted prevention with this group. Men who have sex with men are advised to have an HIV and STI screen at least annually, and every 3 months if having unprotected sex with new or casual partners. Sexual health promotion aimed at the general population should also ensure that a focus on HIV is maintained with the aim of reducing new infections amongst heterosexual people. Other groups vulnerable to increased higher-risk sexual behaviour should also be considered for targeted HIV testing i.e. substance users, sex workers and others engaging in sex with multiple partners (including in public sex environments and via hookup apps). The focus should be flexible to enable targeting to move quickly as new evidence is made available.
Figure 9: Number and percent of late HIV diagnosis, Blackpool
| | Blackpool | North West | England |
|---|
| | Number | % | % | % |
|---|
| 2009-11 |
19 |
31.6 |
52.9 |
50.0 |
| 2010-12 |
14 |
33.3 |
52.4 |
48.4 |
| 2011-13 |
13 |
33.3 |
48.3 |
45.7 |
| 2012-14 |
16 |
38.1 |
46.9 |
43.0 |
| 2013-15 |
16 |
32.7 |
45.7 |
40.2 |
| 2014-16 |
21 |
38.9 |
45.9 |
40.3 |
| 2015-17 |
18 |
34.6 |
43.9 |
41.3 |
| 2016-18 |
21 |
35.6 |
44.6 |
43.1 |
| 2017-19 |
13 |
26.5 |
44.1 |
43.1 |
| Source: PHE, Sexual and Reproductive Health Profiles |
Importantly, we need to increase awareness and uptake of HIV testing by implementing BASHH testing guidance in primary care, ensuring HIV testing is accessible through secondary care, community settings, integrated sexual health services and on-line self-sampling.
Current services
HIV Screening in Accident and Emergency
Blackpool is currently an area of high prevalence and, with a current rate of 4.9 per 100,000, is bordering on extremely high prevalence.
In November 2020, despite being in the middle of the Covid-19 pandemic, Blackpool Teaching Hospital commenced the routine screening of HIV in the Emergency Department (ED), supported by the HIV team. Prior to screening in the ED, and since 2013, HIV screening was offered in the Acute Medical Unit (AMU).
The Emergency Department recorded 10,375 HIV tests in 2021, and this has resulted in seven new HIV diagnoses that may have otherwise remained undetected.
Screening in the community
The National Institute for Health and Clinical Excellence (NICE) has advocated for expanding testing outside clinical settings by engaging community organisations, developing local strategies to increase testing, and by providing rapid HIV tests. Testing in non-medical settings such as community HIV testing, self-sampling and self-testing for HIV broadens the options available to people wishing to take an HIV test.
- The Harm Reduction Service in Blackpool (Renaissance) offers point of care testing within the Blackpool locality, with a focus on MSM.
- HIV home self-sampling enables people across Blackpool to order tests online. Tests are mailed to people's address of choice, with self-taken samples of blood or saliva returned to the provider's laboratory. Confirmatory testing is undertaken by local clinical services for all reactive tests. Home self-sampling screening for a wider range of STIs was introduced by the Blackpool Sexual Health Service prior to the Covid-19 period and became a key part of provision during lockdown periods when in-person attendance was restricted.
National and local strategies
PHE, Trends in HIV testing, new diagnoses and people receiving HIV-related care in the United Kingdom: data to the end December 2019.
PHE, Sexual and Reproductive Health Profiles https://fingertips.phe.org.uk/profile/sexualhealth, (New HIV diagnosis definitions).
PHE, Annual epidemiological spotlight on HIV in the North West, 2019 data.