Infectious and communicable diseases
Last Modified 09/12/2025 10:51:38
Share this page
Note: For COVID-19 specific information for the 2020-2022 period please visit the Coronavirus (COVID-19) summary page.
Introduction
Infectious diseases today continue to pose a significant burden to health and society. The increased mobility of people and goods has contributed to the persistent and ever-changing impact of infectious diseases. Although the effect on mortality of infectious diseases is greater in the developing world, infectious diseases in England generate a significant cost financially, socially, and on health and wellbeing. In the UK, infectious diseases have been estimated to account for half of GP consultations for children, and over a third of GP consultations for adults1.
Public Health England (PHE) leads the surveillance and management of infectious diseases and environmental threats to health through the provision of specialist health protection, epidemiology and microbiology services across England and aims to detect possible outbreaks of disease and epidemics as rapidly as possible. Local Health Protection Teams (HPTs) lead Public Health England's response to all health related incidents and provide specialist support to prevent and reduce the impact of infectious diseases, chemical and radiation hazards and major emergencies.
Health Protection Teams help with:
-
local disease surveillance
-
maintaining alert systems
-
investigating and managing health protection incidents and outbreaks
-
implementing and monitoring national action plans for infectious diseases (Figure 1) at local level
For Blackpool these arrangements are managed by the Cumbria and Lancashire Health Protection Team based in Chorley.
Figure 1: Diseases notifiable to local authority proper officers under the Health Protection (Notification) Regulations 2010
|
Acute encephalitis
|
Diptheria
|
Measles
|
Tetanus
|
|
Acute infectious hepatitis
|
Enteric Fever (typhoid or paratyphoid fever)
|
Meningococcal septicaemia
|
Tuberculosis
|
|
Acute meningitis
|
Food poisoning
|
Mumps
|
Typhus
|
|
Acute poliomyelitis
|
Haemolytic uraemic syndrome (HUS)
|
Plague
|
Viral haemorrhagic fever (VHF)
|
|
Anthrax
|
Infectious blood diarrhoea
|
Rabies
|
Whooping Cough
|
|
Botulism
|
Invasive group A streptococcal disease
|
Rubella
|
Yellow Fever
|
|
Brucellosis
|
Legionnaires' disease
|
Severe Acute Respiratory Syndrome (SARS)
|
|
|
Cholera
|
Leprosy
|
Scarlet Fever
|
|
|
COVID-19
|
Malaria
|
Smallpox
|
|
Source: PHE, Notifiable diseases and causative organisms
Across England and Wales the main notifiable diseases are food poisoning, measles, mumps, scarlet fever, tuberculosis and whooping cough and accounted for over 85% of all notified diseases in 20192.
For information relating to vaccinations, immunisations and other non-communicable health threats see Health Protection.
Facts, figures and trends
Data from PHE's Notifiable Diseases Annual Report shows there were 426 notifications of infectious diseases in Blackpool during the three year period from 2017 to 2019 (Figure 2):
-
215 (50.5%) of the notifications were for scarlet fever. Scarlet fever accounts for just over half of Blackpool's notifications but for only 34.9% of notifications nationally.
-
'Food poisoning' accounted for 16.4% of notifications, similar to 16.6% nationally; a change from the 2012 to 2014 period when 206 notifications (51%) in Blackpool were for food poisoning. This is in part due to increasing classification of campylerbacteriosis and salmonellosis within 'other' infectious diseases. Campylobacteriosis (campylobacter) accounted for 42 (79%) of the 53 'other' notifications in Blackpool between 2017 and 2019, with salmonellosis (salmonella) accounting for a further 2. If taken together, 'food poisoning', campyorbacteriosis and salmonellosis accounted for 114 notifications (26.8%) between 2017-19.
-
Nationally, measles and mumps make up 20.4% of all notifications. In Blackpool, measles and mumps accounted for 56 notifications, 13.1% of all infectious disease notified. Crude rates for laboratory confirmed infection for measles in 2018 were below the national average at 0.7 per 100,000 compared to the England average of 1.7. Similarly the 2018 rate for mumps in Blackpool was 0.7 per 100,000, compared to the England average of 1.9.
-
There were 25 tuberculosis notifications, 5.9% of all notified diseases.
-
No notifications of meningococcal septicaemia were made in Blackpool during the 2017 to 2019 period.
Figure 2: Notifications of infectious diseases by disease group: Blackpool and England & Wales, 2017 to 2019
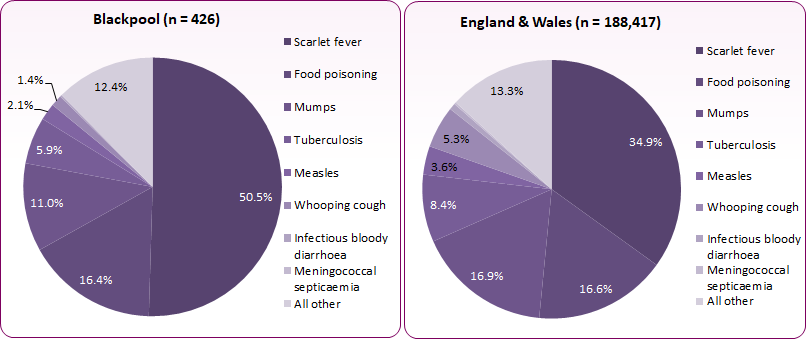 Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019
Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019
The causes, patterns and effects of infectious diseases are determined by an interplay of numerous factors related to the individual (age, sex, health, immunity, and behaviour), the pathogen, and the environment (climate, air quality, socio-economic)3. Figure 3 shows the rate of all notifications of infectious diseases by age group across England and Wales. The chart shows an overall higher rate for younger children (0 to 9 years), mainly due to higher levels of scarlet fever and measles amongst this age group.
Figure 3: Notifications of infectious diseases by age group, crude rate per 1,000 population: England & Wales, 2017-19
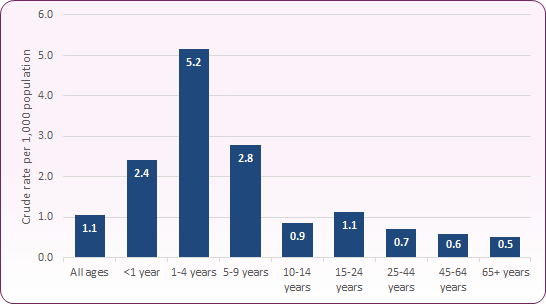 Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019; ONS mid-year population estimates, 2017, 2018, 2019.
Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019; ONS mid-year population estimates, 2017, 2018, 2019.
The key issues in relation to infectious diseases and/or agents that constituted the highest rates of notifications from Blackpool in 2017-19 included:
-
-
Scarlet fever is a bacterial illness that mainly affects children and causes a distinctive pink-red rash. The current national rise is reflected locally with 215 notifications between 2017 and 2019. In 2016, there were 107 notified cases of scarlet fever in Blackpool (97 in children aged 0-9 years, the second highest rate in the England at 589 per 100,000). Whilst recent years have seen fewer cases (56 in 2019), levels remain relatively high compared to before 2014.
-
-
Food poisoning is an illness caused by eating contaminated food. It's not usually serious and most people get better within a few days without treatment, though some infections can cause long-term and severe health problems in some, including young children and the elderly4. Food poisoning notifications recorded in Blackpool are lower than the 2011-13 period, when there was an average of 78 notifications per year: notifications for food poisoning, campylobacteriosis and salmonellosis averaged 38 per year between 2017 and 2019.
-
Measles is a viral illness that can lead to serious complications, and is a vaccine preventable disease. 9 cases were reported between 2017 and 2019, with levels having been relatively steady in Blackpool since 2013.
-
Mumps is also a viral illness which is vaccine preventable. Mumps is now more common, particularly in young adults who were not fully vaccinated against mumps in childhood and who have not been exposed to naturally occurring illness. Across Blackpool there were 47 notifications of mumps between 2017 and 2019, including 30 notifications in 2019.
-
Tuberculosis accounted for 25 infectious disease notifications, 8.4% of all Blackpool's notifications in 2017 to 2019. Infections are showing a downward trend from the 2012-14 period when there were 55 notifications.
-
Infectious bloody diarrhoea, meningococcal septicaemia and whooping cough accounted for only 1.6% (7) of notifications in Blackpool in 2017-19 compared to 6.3% nationally. Whooping cough makes up 5.3% of notifications in England and Wales but only 1.4% in Blackpool.
-
Children aged under 5 years have the highest rate of notifications out of all age groups followed by children aged 5-9 years (Figure 3). Scarlet fever, measles, mumps and food poisoning are the main diseases notified for these age groups.
Scarlet fever
Scarlet fever is a common childhood infection caused by Streptococcus pyogenes. Once a dangerous disease in the UK, antibiotic treatment has now meant that scarlet fever is much less serious. Cases of scarlet fever occur through the year but have a seasonal pattern with highest incidence between December and May5.
Levels of scarlet fever have risen across England and Wales since 2014, and this rise is reflected in Blackpool notifications (Figure 4).
Figure 4: Number of notifications of scarlet fever in England & Wales, the North West and Blackpool
| Scarlet fever | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|
| England & Wales |
2719
|
4254 |
4643 |
15637 |
17696 |
19206 |
17813 |
31904 |
16128 |
|---|
| North West |
311
|
727 |
741 |
2211 |
2284 |
2724 |
2834 |
5414 |
2691 |
|---|
| Blackpool |
9
|
5
|
17
|
41
|
79
|
107 |
75 |
84 |
56 |
|---|
Source: PHE, Notifiable Diseases Annual Report 2011-2019
Tuberculosis (TB)
Tuberculosis is a bacterial infection spread through inhaling tiny droplets from the coughs or sneezes of an infected person. It mainly affects the lungs. However, it can affect any part of the body, including the glands, bones, and nervous system. TB that affects the lungs is the most contagious type, but it usually only spreads after prolonged exposure to someone with the illness. For example, it often spreads within a family who live in the same house. TB re-emerged as a serious public health problem in the UK over the last two decades.
-
-
Across Blackpool the incidence of TB notifications rose between 2003-05 and 2010-12 to a point comparable to the England average rate (Figure 5). From 2011-13 the rate has steadily fallen nationally, regionally and locally. In the three year period 2017 to 2019, Public Health England reported a TB incidence rate for Blackpool of 5.3 per 100,000 population, compared to a rate of 8.6 for England.
Figure 5: Trend in incidence of TB notifications, Blackpool compared to England and the North West
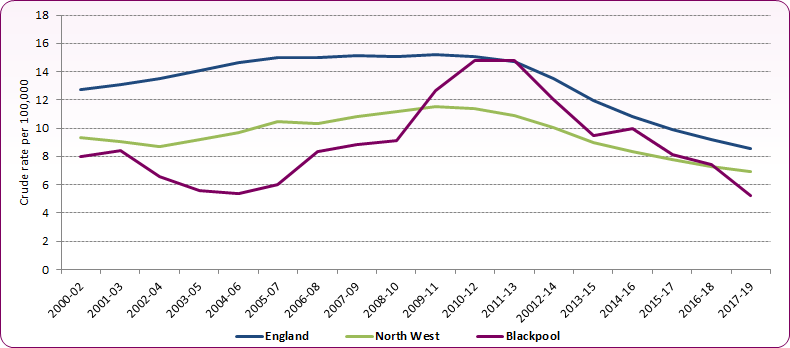 Source: PHE, Public Health Profiles
Source: PHE, Public Health Profiles
Timely and fully completed treatment for TB is key to saving lives and preventing long-term ill health, as well as reducing the number of new infections and development of drug resistance. Dropping out of treatment before it is completed can contribute to drug-resistant TB, and preventing the development of drug resistant TB is particularly important as it has more severe health consequences and is considerably more difficult to treat.
Measles and mumps
Measles is a highly infectious viral illness that can be very unpleasant and can sometimes lead to serious complications. However, it is now relatively uncommon in the UK because of the effectiveness of the MMR vaccination. Mumps is a contagious viral infection that used to be common in children before the introduction of the MMR vaccine.
Figure 6: Number of notifications of measles in England & Wales, the North West and Blackpool
| Measles | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|
| England & Wales |
2,355
|
4,211
|
6,193
|
1,850
|
1,193
|
1,641 |
1,693 |
2,608 |
2,422 |
|---|
| North West |
203
|
1,491
|
1,228
|
296
|
197
|
176 |
276 |
352 |
324 |
|---|
| Blackpool |
5
|
7
|
5
|
5
|
3
|
1 |
5 |
1 |
3 |
|---|
Source: PHE, Notifiable Diseases Annual Report 2011-2019
The success of the MMR vaccine means that cases of measles are uncommon in the UK. However, the number of cases has risen in recent years and there have been some high-profile outbreaks. For example, between November 2012 and July 2013 there was a measles outbreak in and around Swansea, during which more than 1,200 cases were reported. It is thought that the rise in the number of cases of measles is largely due to parents not getting their child vaccinated with the MMR vaccine, probably due to inaccurate research linking MMR to autism.
Figure 7: Number of notifications of mumps in England & Wales, the North West and Blackpool
| Mumps | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | 2019 |
|---|
| England & Wales |
6,888
|
7,530
|
10,095
|
8,338
|
6,114
|
5,160 |
7,723 |
6,749 |
17,309 |
|---|
| North West |
864
|
1,226
|
1,384
|
869
|
747
|
597 |
886 |
1,579 |
3,087 |
|---|
| Blackpool |
12
|
24
|
20
|
9
|
5
|
3 |
10 |
7 |
30 |
|---|
Source: PHE, Notifiable Diseases Annual Report 2011-2019
Mumps cases nationally continue to be identified predominantly in young adults between 16 and 30 years of age, with 68.6% of notifications in 2019 being amongst those aged under 25 years. The recent rise in cases has mainly been driven by outbreaks in universities and colleges, with many of the cases in 2019 seen in so-called 'Wakefield cohorts', born in the late 90's and early 2000's who missed out on the MMR vaccine when they were children6.
The above trends are reflected in the 2017-2019 age distribution of notifications for measles and mumps in England and Wales (Figure 8), with 76% of measles notifications occuring in those aged under 9 years, and 40.5% of mumps notifications occuring in those 15 to 24 years.
Figure 8: Proportions of mumps and measles notifications by age group, England and Wales 2017-2019
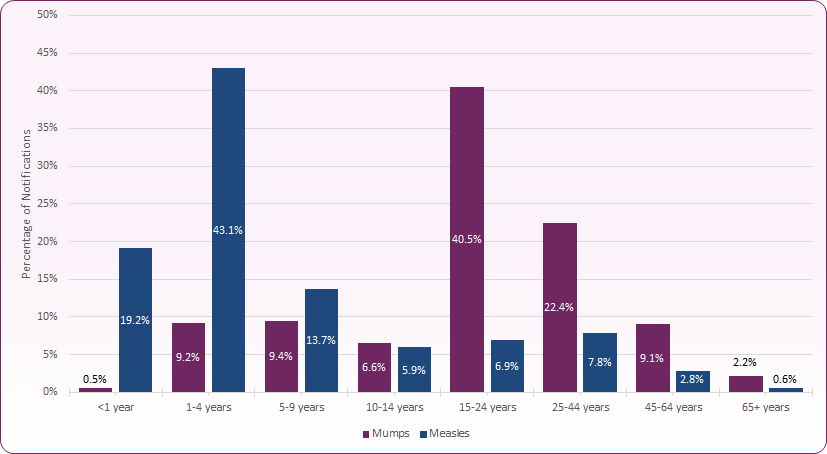 Source: PHE Notifiable Diseases Annual Report 2017, 2018, 2019.
Source: PHE Notifiable Diseases Annual Report 2017, 2018, 2019.
Food poisoning and associated pathogens
Food poisoning is an illness caused by eating contaminated food. It's not usually serious and most people get better within a few days without treatment. In most cases of food poisoning, the food is contaminated by bacteria, such as campylobacter (the most common bacteria causing food poisoning in the UK), salmonella or Escherichia coli (E. coli), or a virus, such as the norovirus.
Food poisoning is one of the most common causes of gastroenteritis in adults. The most common cause of gastroenteritis in children is rotavirus. This virus is passed out in the stools (faeces) of someone with the infection. It can be transferred to food, objects and surfaces if the infected person doesn't wash their hands after going to the toilet.
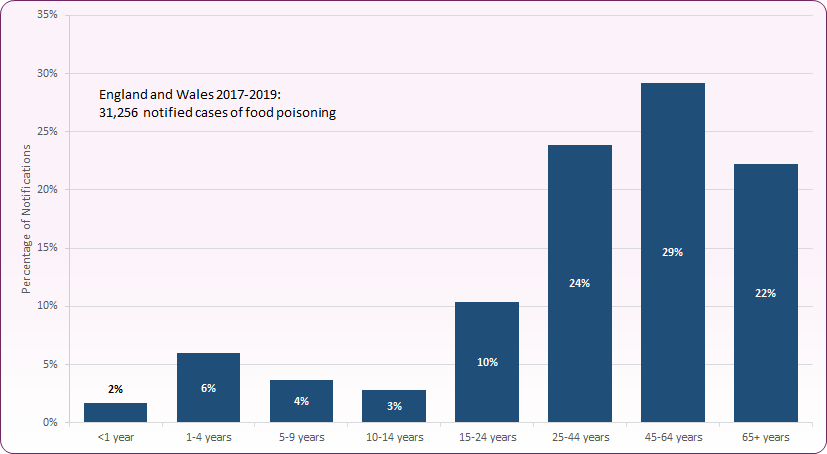
England and Wales notification data shows that three quarters (75%) of notifications for food poisoning in 2017 to 2019 were amongst those aged over 25 years (Figure 9)7.
Figure 9: Proportion of food poisoning notifications by age group, England & Wales, 2017 to 20197
 Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019.
Source: PHE, Notifiable Diseases Annual Report, 2017, 2018, 2019.
Until recently there has been little local data about different types / causes of food poisoning, however over the last three years there has been increasing notification recording of causative agents such as campylobacter and salmonella. 2019 notifications for Blackpool identified 21 reports of 'food poisoning', 26 of campylobacter and 7 other pathogens that may be associated to food / drink poisoning (but can also be transmitted through other routes). Together these represented 35% of all infectious disease notifications for the year.
Risk factors
The key demographic change to impact on the incidence of communicable diseases is travel and migration. Not only can this affect the incidence of diseases such as TB and hepatitis B but may increase the risk of pandemic infections. In addition, vaccination programmes are different in different countries and children entering the country may not have completed the UK immunisation schedule.
Prevention
Many infections are easily preventable by healthcare partners but require vigilance to prevent infections carried by food, water, infected objects, excreta, bodily fluids and droplets. Essential practices for preventing infection encompassing all the determinants of health include:
-
-
handwashing which hugely reduces infection spread in every setting, especially in clinical situations and after contact with animals and soil.
-
breastfeeding maximises infant immunity to infections, including gastroenteritis.
-
good nutrition improves immune function.
-
adequate hydration helps prevent urinary tract infections in elderly.
-
appropriate vaccinations (See childhood and adult immunisation).
-
adequate housing with sufficient space prevents spread of infections, for example TB.
-
good thermal insulation and adequate heating prevent respiratory infections and excess winter deaths.
-
early diagnosis, treatment, and isolation when necessary and rapid referral prevent infections spreading.
-
education, monitoring and regulation to maintain vigilance on these essential actions to prevent infection.
Infection control must be a priority. Without infection control all other activity to promote health and wellbeing can be swiftly undermined when an outbreak occurs and large numbers of people are affected. Ongoing vigilance is required as antibiotic resistance increases (for example the global epidemic of multi-drug resistant TB, currently prevalent in London) reducing the armoury of drugs available for control. The aim should be targeted prevention using infection control frameworks including the screen, treat and immunisation roles of occupational health for TB, measles, Hepatitis C, and healthcare acquired infections (HCAI).
National and local guidance
'Notification of infectious diseases' is the term used to refer to the statutory duties for reporting notifiable diseases in the Public Health (Control of Disease) Act 1984 and the summary of health protection legislation supports the management of outbreaks and incidents.
Health Protection (Notification) Regulations 2010.
The elimination of TB has been identified as a key priority by the UK Health Security Agency (UKHSA), working with NHS England, and the Tuberculosis (TB) Action Plan for England, 2021-26 outlines plans to improve prevention, detection and control of TB in England.
Current NICE guidelines (NG33) Tuberculosis (2024) cover preventing, identifying and managing active and latent TB in children, young people and adults.
National Measles Guidelines from PHE on how to manage cases of suspected measles include what patient details to take; who to notify and assessing risk of disease spreading in close contacts.
Mumps guidance, data and analysis provide information on symptoms, diagnosis, management, surveillance and epidemiology of mumps.
[] Brownlie J. et al. Foresight. Infectious Diseases: preparing for the future, Future Threats. Office of Science and Innovation, London (2006)
[] Source: PHE, Notifiable diseases annual report, 2019
[] UK Trends in Infectious Diseases, Houses of Parliament, Parliamentary Office of Science and Technology, Postnote 545, January 2017.
[] For further information about specific bacterial and viral causes of food poisoning, see Food Standards Agency website.
[] UKHSA, Guidelines for the public health management of scarlet fever outbreaks in schools, nurseries and other childcare settings
[] PHE, Mumps Outbreaks across England, February 2020.
[] Note: this does not include specific notifications of campylobacter, salmonella, E.coli or other pathogens that may cause food poisoning since age breakdown was not available for these notifications at time of publication.