Childhood Immunisations (5 years and over)
Last Modified 10/07/2025 14:14:47
Share this page
Introduction
After clean water, vaccination is the most effective public health intervention in the world for saving lives and promoting good health. Immunisation is the most essential way of protecting people and communities from serious infectious diseases. As well as the individual being protected themselves, vaccinated people are also less likely to be a source of infection to others.
Many vaccine-preventable childhood diseases are now so rare that it is easy to underestimate the importance of children's vaccinations. However, whooping cough and diphtheria are still a threat. The diseases are rare now, but if children are not vaccinated, they can return with a vengeance.
Currently the European Region of the World Health Organization (WHO) recommends that on a national basis at least 95% of children are immunised against diseases preventable by immunisation and targeted for elimination or control (specifically, diphtheria, tetanus, pertussis, polio, Hib, measles, mumps and rubella)1. The routine childhood immunisation programme for the UK includes these immunisations recommended by WHO as well as a number of others as defined by the UK Health Security Agency (UKHSA). The complete routine immunisation schedule is published annually by the UK Health Security Agency.
Childhood immunisations (0-4 years) and adult vaccinations provides data on younger children and adults. Further information on infectious diseases and other noncommunicable health threats is available in the Health Protection section.
Facts, figures and trends
In addition to the Department of Health and Social Care, Health Protection Profile, vaccination coverage data can be accessed via an experimental interactive dashboard:
Note: The COVID-19 period has impacted vaccination and immunisations programmes in a number of ways. During the COVID-19 period, coverage for some vaccinations dropped across the country, for example in relation to measles, mumps and rubella (MMR) vaccination. The UK Heath Security Agency has warned that susceptibility will have increased in recent years, with the potential for larger outbreaks.
2023/24 data published by NHS England shows that in Blackpool:
-
- The number of children who had received the Haemophilus influenza type b and meningitis C (Hib/MenC) booster by age 5 years was 1,710 (91.9%)
- The number of children who received the combined Diptheira, Tetanus, Polio, Pertussis, Hib and HepB primary vaccine by age 5 year was 1,747 (93.9%)
- The number of children who received the combined Diptheira, Tetanus, Polio and Pertussis booster vaccine by age 5 year was 1,568 (93.9%)
- The number of children who had received the measles, mumps and rubella (MMR) vaccine, 1 dose, by age 5 years was 1,740 (84.3%)
- The number of children who had received the measles, mumps and rubella (MMR) vaccine, 2 doses at age 5 years was 1,604 (86.2%)
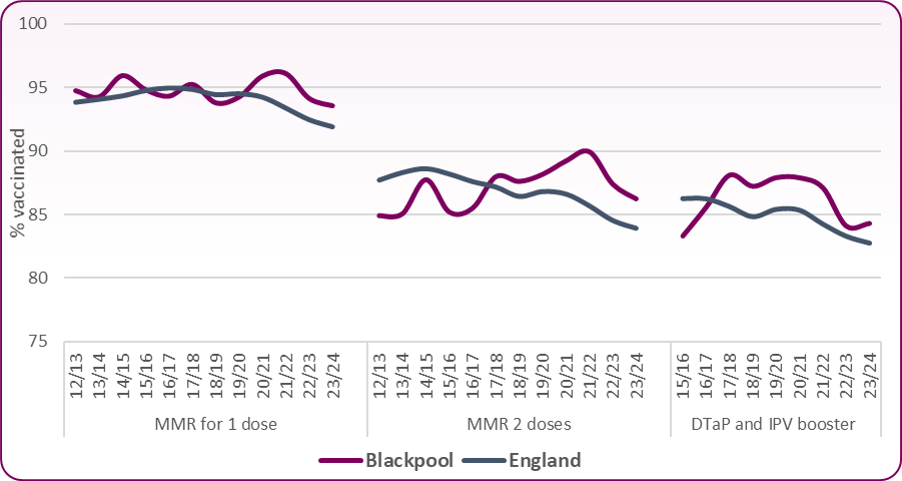
Figure 1: Percent of children immunised by their 5th birthday: 2023/24
 Source: NHS England, Childhood Vaccination Coverage Statistics: Data Tables
Source: NHS England, Childhood Vaccination Coverage Statistics: Data Tables
Figure 2: Trend in proportion of children immunised by their 5th birthday
 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Across Blackpool, immunisation uptake by the age of 5 years is higher than the national average but recent trends show uptake is falling locally and nationally. Two doses of MMR vaccine are required to provide satisfactory protection against measles, mumps and rubella, and although coverage in Blackpool is above the national average (Figure 1) it remains below the goal of 90%. In 2023/24, 86.2% of Blackpool's children had two doses of the MMR vaccine by the time they began school, a continuing fall on the previous years. Approximately 5%-10% of children are not fully immune after only one dose of the vaccine, therefore the second dose provides a further opportunity to protect children, with less than 1% of children remaining susceptible after receiving the two recommended doses2.
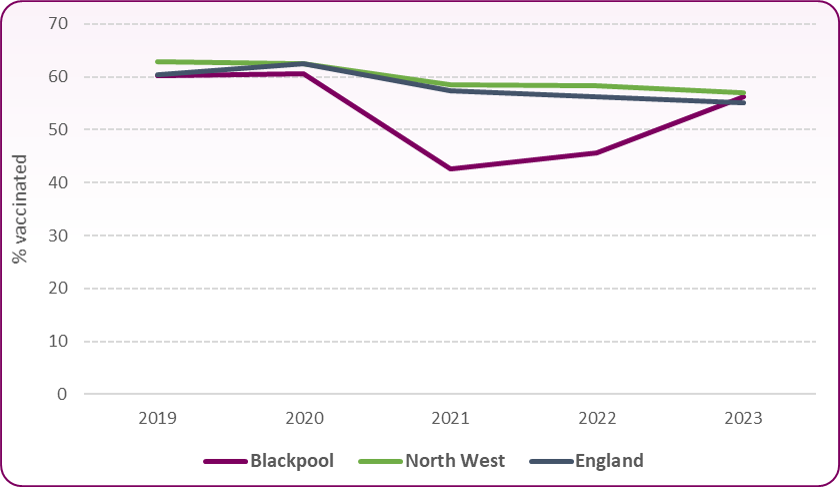
Figure 3 shows the longer term trend in the proportion of children who have received two doses of the MMR vaccine by their 5th birthday. In Blackpool coverage has increased from lower than the national average before 2019/20 to higher than average, though in recent years coverage has been falling nationally, regionally and locally.
Figure 3: Trend in the proportion of children who have 2 doses of MMR vaccine by their 5th birthday
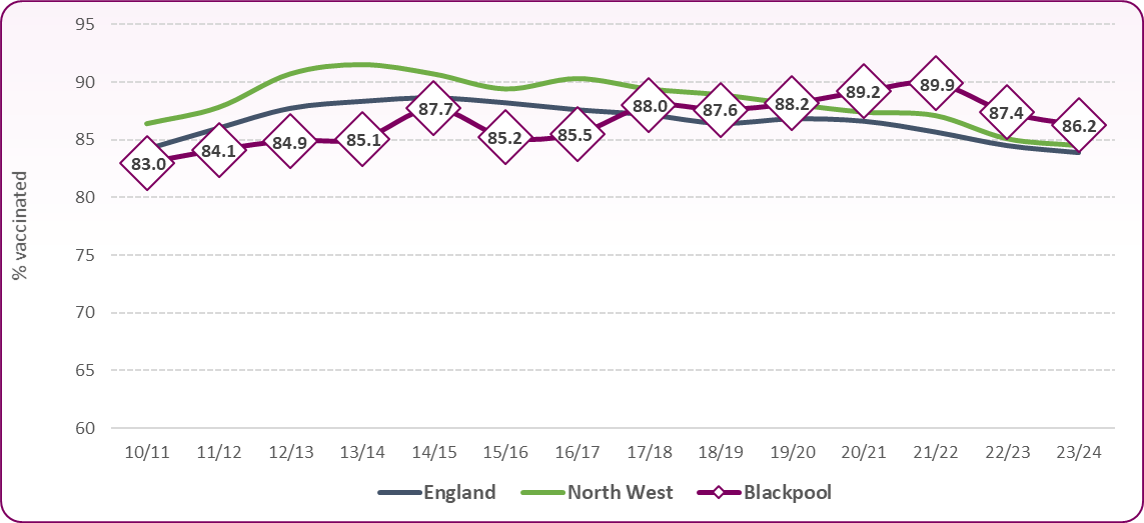 Source: OHID, Health Protection Profile, Immunisation and childhood vaccine preventable diseases
Source: OHID, Health Protection Profile, Immunisation and childhood vaccine preventable diseases
Figure 4 compares Blackpool with other local authorities in England. Blackpool ranks 69th out of 148 authorities with reported statistics and is in the third (middle) quintile for coverage.
Figure 4: Proportion of children who have 2 doses of MMR vaccine by their 5th birthday, comparison showing Blackpool with upper tier local authorities in England, 2023/24
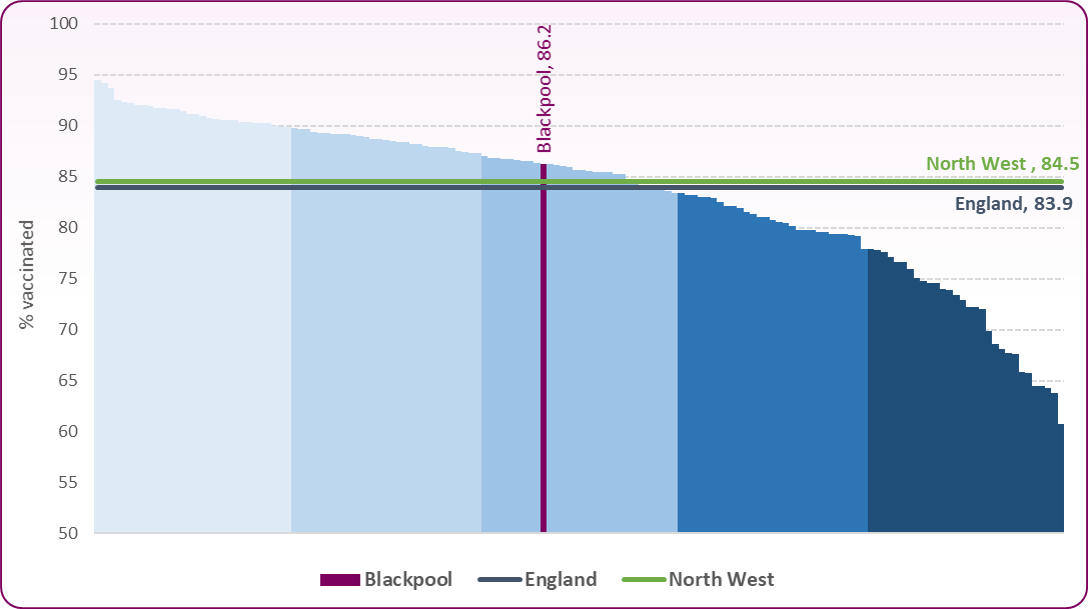 Source: OHID, Health Protection Profile, Immunisation and childhood vaccine preventable diseases
Source: OHID, Health Protection Profile, Immunisation and childhood vaccine preventable diseases
National data reported that there were 173 lab-confirmed cases of mumps in England in 2023, compared to 17 cases in 2021 and 367 cases of measles, up from just 2 in 2021. Outside of London, the risk of measles is low but smaller outbreaks could be seen in specific populations, including teenagers, young people and under-vaccinated communities and it highlights the importance of ensuring that children are up-to-date with the MMR vaccination3. Following the increases in measles, the UK Health Security Agency (UKHSA) launched a campaign in March 2024 to remind parents of the risks of their children missing out on protection against serious disease.
The HPV vaccine protects against two types of HPV virus (HPV-16 and HPV-18) which together are responsible for about 70% of cervical cancers. In addition, the vaccine can also protect against HPV-6 and HPV-11, the two strains of HPV that cause most cases of genital warts.
Since 2008, all 12 to 13 year old females (school year 8) in the UK have been offered the human papilloma virus (HPV) vaccination through the national HPV immunisation programme. From the 2019/20 school year, HPV vaccination was also extended to males aged 12 to 13. Following updated guidance in 2023, the NHS have now updated its HPV vaccination programme to a single dose instead of two doses for most under 25s, making it easier than ever for young people and parents of 12-13 year olds to ensure they are protected.
In 2023, the NHS also pledged to eliminate cervical cancer by 20404 for the first time ever, which could save thousands of lives every year in England, but this relies on as many young people as possible getting the lifesaving HPV vaccination and increasing cervical screening uptake.
Due to the COVID-19 pandemic, all educational settings were closed from the 23 March 2020 and the delivery of the 2019/20 school immunisation programmes was paused, in line with UK Government COVID-19 guidance. This has had a significant impact on the uptake of the HPV vaccination programme. Latest figures overall indicate that uptake is stabilising, with encouraging signs of increases when people are first offered the vaccine in year 8. However, HPV vaccine uptake among school pupils is still well below pre-pandemic levels of around 90%.5
In Blackpool in 2022/23:
-
- 75.1% (538) of girls aged 12 to 13 years received their first dose vaccination for HPV compared to 81.8% in 2019/20 (pre pandemic)
- 69.6% (489) of girls aged 13 to 14 years received their second dose vaccination for HPV compared to 83.8% in 2019/20
- 63.9% (488) of boys aged 12 to 13 years received their HPV vaccination compared to 77.6% in 2019/20
In Covid-affected 2020/21:
-
- 72.4% (501) of girls aged 12 to 13 years received their first dose vaccination for HPV
- 80.1% (520) of girls aged 13 to 14 years received their second dose vaccination for HPV
- 64.7% (467) of males aged 12 to 13 years received their first dose vaccination for HPV
Currently, coverage for girls is higher than national and regional averages (Figure 5) but significantly below the 80% uptake target. For boys, uptake is below the national average of 65.2% and also significantly below the 80% target. Until the Covid impact, vaccination coverage in girls had been relatively stable and above the 80% target for both one and two doses (Figure 6).
Figure 5: Proportion of children aged 12-13 and 13-14 receiving HPV vaccine 2022/23
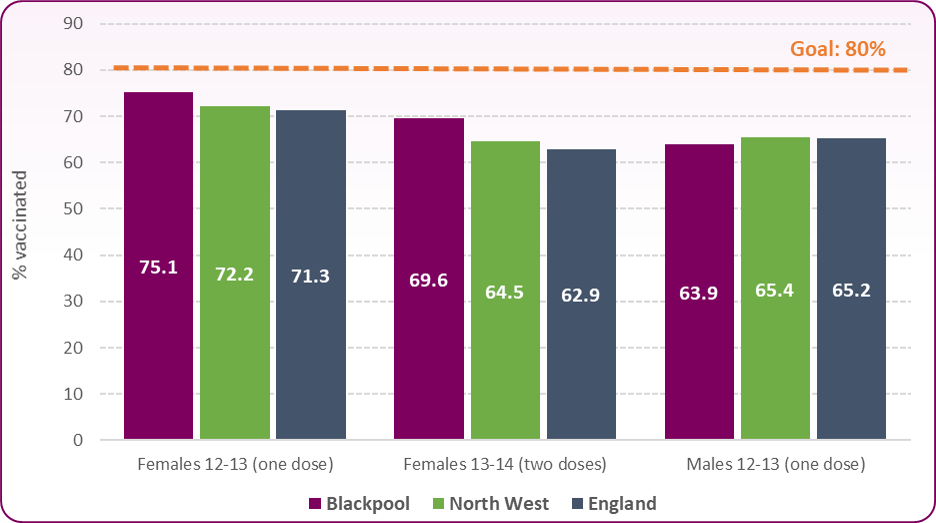 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Figure 6 : Trend in proportion of females and males aged 12-13 (one dose) and females aged 13-14 (two doses) receiving HPV vaccine
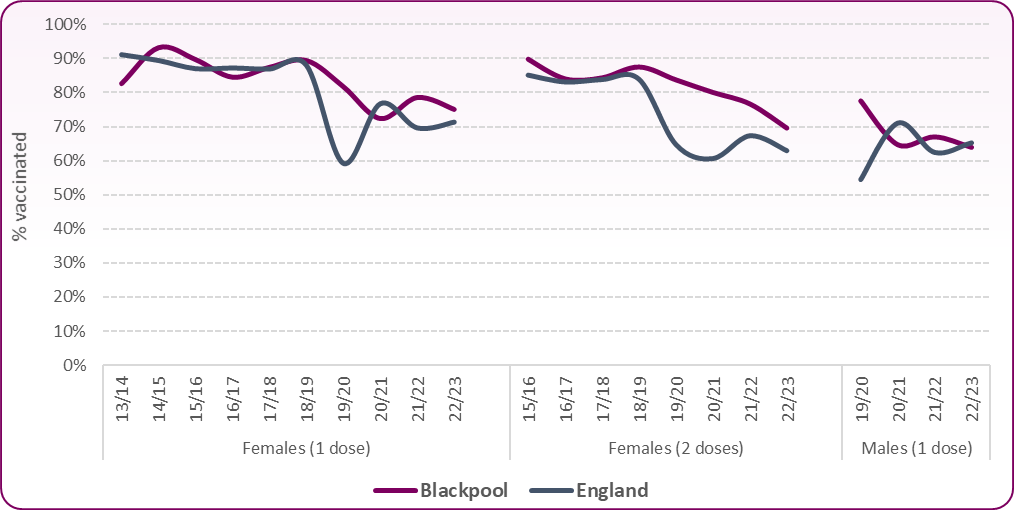 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Influenza
In 2012 the Joint Committee on Vaccination and Immunisation (JCVI) recommended that the flu vaccination programme should be extended to all children aged two to 16 years old. The phased introduction of the programme to children began in 2013/14 and all primary school-aged children were offered the vaccine from the 2019/20 season onwards. The national ambition for the 2023/24 flu season was to demonstrate a 100% offer and to achieve at least the uptake levels of 2022/23 (which across England was 43.7%)
In 2023/24
-
- 1,169 (34.4%) 2-3 year old children in Blackpool received a flu vaccination compared to 37.1% the previous year
- 56.2% of primary aged children received a flu vaccination compared with 45. 6% last year (Figure 7)
Figure 7: Influenza Vaccination Coverage Trend (Primary School ages 4 to 11)
 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Variation within Blackpool
At a local level, there is variation in the proportion of children immunised in each of Blackpool's GP practices, with several practices having rates significantly lower than the Blackpool average. Figure 8 shows immunisations by the age of 5 years and the proportion of children immunised by each practice in 2023/24.
Figure 8: Child Immunisations by the age of 5 years by GP Practice in Blackpool, 2023/24
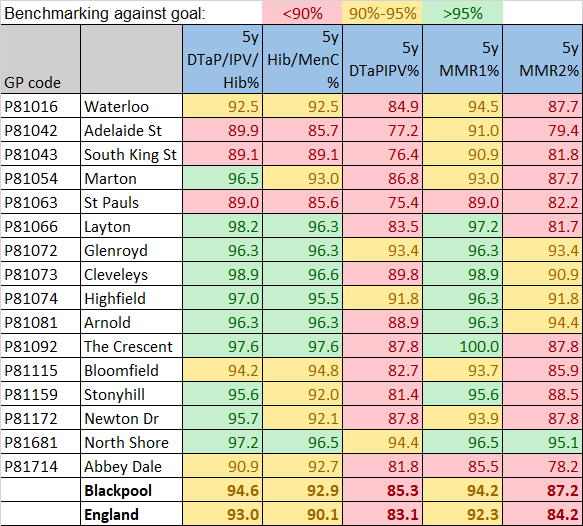 Source: NHS England, Child Immunisation by GP Practice
Source: NHS England, Child Immunisation by GP Practice
In recent years there has been a renewed focus on improving outcomes for looked-after children and young people who can be at a higher risk of missing out on childhood vaccinations. Looked after children in Blackpool are significantly more likely to be up to date with their immunisations: in 2023, 93% of children in care for at least 12 months had all their immunisations compared to 82% nationally.
Risks
Reasons for low uptake of vaccinations may include poor access to healthcare services; inaccurate claims about safety and effectiveness, which can lead to increased concerns and a reduction in the perceived need for vaccines; and insufficient capacity in the healthcare system to provide vaccinations. In addition, problems with the recording of vaccination status and poor identification of people who are eligible to be vaccinated may have contributed to low uptake6.
Blackpool recognises that there is a need to target both overall improvement of immunisation coverage and specifically to improve the low levels of coverage amongst certain groups and in certain places.
Evidence has shown that the following groups of children and young people are at risk of not being fully immunised6:
-
- People from some minority ethnic family backgrounds
- People from Gypsy, Roma and Traveller communities
- People with physical or learning disabilities
- People from some religious communities (for example, Orthodox Jewish)
- New migrants and asylum seekers
- Looked-after children and young people
- Children of young or lone parents
- Children from large families
- People who live in an area of high deprivation
- Babies or children who are hospitalised or have a chronic illness, and their siblings
- People not registered with a GP
- People from non-English-speaking families
- People who are homeless
Vaccine hesitancy
In recent years, vaccine hesitancy has been on the rise with more people questioning vaccination as anti-vaccine messages have been amplified on social media. As a result, vaccine hesitancy is slowly chipping away at the eradication achieved for various infectious diseases, including polio and measles.
In 2023 around 70% of UK adults said that vaccinations were safe and effective, down sharply from 90% in 2018, according to research from the Vaccine Confidence Project, run by the London School of Hygiene and Tropical Medicine (LSHTM). At the same time, childhood vaccination rates have fallen further below recommended levels over the last five years, continuing a longer-term trend7.
Mitigating vaccine hesitancy is crucial for public health, and there are several strategies that can help:
-
- Improving Public Trust in Vaccines
- Fostering Education and Awareness
- Engaging with Communities
- Improving Access and Convenience
- Addressing Specific Concerns
It’s important to take a holistic approach that involves communication, education, accessibility, and empathy so that vaccine hesitancy can be addressed more effectively.
National and local strategies
Department of Health (2024) immunisation information for health professionals and immunisation practitioners
The 'Green Book' has the latest information on vaccines and vaccination procedures, for vaccine-preventable infectious diseases in the UK.
The Complete Immunisation Schedule in the UK includes the ages of when the vaccines should be given.
NICE guideline [NG218] Vaccine uptake in the general population, May 2022 aims to increase the uptake of all vaccines by everyone who is eligible. It supports the aims of the NHS Long Term Plan, which includes actions to improve immunisation coverage by GPs and support a narrowing of health inequalities.
NHS England’s NHS vaccination strategy (January 2024) is for people and organisations involved in the commissioning, planning and delivery of NHS vaccination services in England and will aim to not only increase overall uptake and coverage of vaccinations, but to reduce disparity in uptake.
[] WHO Regional Office for Europe, European Immunization Agenda 2030, 2021
UKHSA, The Green Book of Immunisation, Chapter 21, December 2019
UKHSA, Laboratory confirmed cases of measles, rubella and mumps in England, May 2024
[] NHS England, NHS sets ambition to eliminate cervical cancer by 2040, November 2023
[] UKHSA, Young people urged to catch-up on missed HPV vaccines, January 2025
[ NICE guideline [NG218] Vaccine uptake in the general population, May 2022
] BBC Indepth, Rise of vaccine distrust - why more of us are questioning jabs, January 2025 [Accessed 26/02/2025]