Drug Misuse
Last Modified 14/02/2024 15:34:59
Share this page
Introduction
Drug misuse is a major concern, both locally and nationally, causing harm to individuals, families and communities. Harms from drug misuse cost society an estimated £9.3 billion per year, 86% of which is attributable to the health and crime-related costs of the heroin and crack cocaine markets. Drug deaths are at the highest level on record, and since 2012 heroin-related deaths have more than doubled and deaths involving cocaine have increased five-fold. The highest rates of opiate and crack use are seen in the North of the country and in the most deprived areas1.
Blackpool addresses the substance misuse needs of the population through a range inter-related strategies and services. In addition to adult drug misuse needs outlined below, please also see the following:
The Prevalence of Drug Use in England and Blackpool
It is not possible to measure the prevalence of drug use across the UK accurately. Prevalence estimates are generated from a range of sources in order to gain a general understanding of patterns of use nationally, regionally and locally.
The ONS Crime Survey for England and Wales (CSEW) is the primary means of estimating drug use prevalence. The 2020 survey (ending March 2020)2 found that:
-
There was no change in overall use and Class A3 drug use in the previous year across England and Wales
-
An estimated 3.2 million (9.4%) adults aged 16 to 59 had taken an illicit drug in the previous year
-
Adult men were nearly twice as likely as women to have reported using a drug in the last year
-
Reported drug use was highest among those in a low income household (less than £10,400 pa), though similar across other income groups
-
21% of adults aged 16 to 24 had taken a drug in the previous year
-
Full-time students (19.7%) were more likely than any other occupational group to have used a drug in the previous year
-
1% of adults aged 60 to 74 had taken a drug in the previous year
-
3.4% of adults aged 16 to 59, and 7.4% of adults aged 16 to 24, had taken a Class A drug in the previous year
-
2.1% of adults aged 16 to 59 and 4.3% of adults aged 16 to 24 were classed as “frequent” drug users (taking a drug more than once a month in the previous year)
-
Cannabis is the most commonly used drug, with 7.8% of 16 to 59s and 18.7% of 16 to 24s using the drug in the previous year
-
Powdered cocaine was the second most commonly used drug among 16 to 59s (2.6%), whilst nitrous oxide was the second most commonly used drug among 16 to 25s (8.7%)
Drug use prevalence varies by age group, with younger age groups having higher levels of overall drug use prevalence (any illicit substance) (Figure 1). Whilst drug use prevalence among over 30s has remained relatively stable following declines between 2001/02 and 2012/13, estimated use among under 30s has risen over the past ten years. This appears to be primarily due to increases in cannabis and powdered cocaine use. Estimated cannabis prevalence among 20 to 24 year olds increased from 13% in 2012/13 to 18.3% in 2019/20, and estimated powdered cocaine prevalence rose from 3.7% to 6.1% over the same period (though has reduced from 8% over the last two years).
Figure 1: CSEW Estimated Drug Prevalence by Age Group, England and Wales 2001/02 to 2019/20
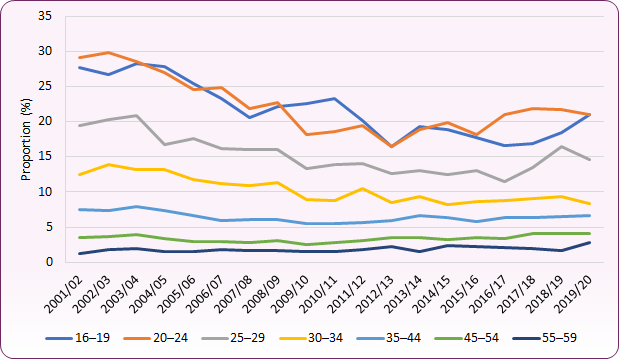 Source: Office for National Statistics, Drug Misuse Appendix Tables: Finding from the year ending March 2020 Crime Survey for England and Wales.
Source: Office for National Statistics, Drug Misuse Appendix Tables: Finding from the year ending March 2020 Crime Survey for England and Wales.
ONS regional estimates suggest that in North West England for the year up to March 2020:
-
9.1% of adults aged 16 to 59 had taken a drug in the previous year. The highest estimated rates were in the South West (12%) and London (10.9%)
-
3.6% of adults had taken a Class A drug (the highest rate outside London and the South of England)
-
3.1% of adults had taken powdered cocaine (the highest rate outside London), and an increase from 2.2% in 2015-2016
-
Estimated prevalence rates for all substances (except amphetamines) in 2019-20 are lower than 2018-19 estimates, but generally higher than the 2015-16 / 2016-17 period.
Coronavirus and Drug Prevalence Measurement
The 2020 CSEW was suspended on the 17 March 2020 and estimates are largely unaffected by the coronavirus (COVID-19) pandemic. For the COVID-19 period the CSEW was adapted for telephone-operated delivery to a smaller sample group (TCSEW). The survey reported that 6.5% of those aged 18 to 59 and 15% of those aged 18 to 24 reported taking a drug in the last year. Due to the changes in methodology this is not comparable with previous trends and the 2020 data is regarded as more reliable.
There are, however, suggestions that COVID-19 lockdown periods altered patterns of drug use, both as a consequence of changes to behaviour during lockdown and because of the impact on global supply chains. A 2020 survey by Release5 suggested, for example, that there may have been reduced use of MDMA / ecstasy during the COVID-19 period (due to restrictions on night-time economy / social activity), whilst cannabis use was common. The report also suggested that as well as harms from coronavirus itself, the COVID-19 period brought additional risks for some people who use drugs, with increased frequency of (non-fatal) overdose, withdrawal problems, increased police contact, and the sharing of injecting equipment.
Opiate and Crack Use Prevalence in Blackpool
Local prevalence data is not available from the CSEW. However, for the 2019/20 period, the Office for Health Improvement and Disparities and the UK Health Security Agency have estimated the number and prevalence of opiate and/or crack cocaine use (OCU) based on revised methodology.4 Information about OCU is an essential part of the evidence base to help plan services to tackle opiate and crack dependence. OCU does not include the use of cocaine in powder form, amphetamine, ecstasy or cannabis.
In 2019/20, 2,468 people (aged 15-64) were estimated to be using opiate and/or crack cocaine in Blackpool, a crude rate of 28.6 per 1,000 population. This compares to a rate of 9.5 per 1,000 for England and 11.9 per 1,000 for the North West. Blackpool’s estimated OCU rate was the third highest in the country after the City of London (56.8) and Middlesbrough (31.3), and remains the same as the previous estimate in 2018/19.
For opiate use only it is estimated there were 1,182 opiate users in Blackpool (2019/20) at a rate of 13.7 per 1,000 population, and the fifth highest in the country. There were an estimated 310 crack cocaine users, at a rate of 3.6 per 1,000 population (fourth highest in country). Drug treatment data in itself is not a reliable measure of prevalence, however service data suggests that since 2016-17 there has been a slight increase in opiate users also using crack cocaine (and a reduction in opiate users not using crack cocaine). This may be indicative of a changing trend in use.
Drug Offences Among Over-25s in Blackpool
Police recorded drug offences may not be a reliable measure of overall drug prevalence since they take place within a specific legislative framework, are subject to particular policing strategies and resources (e.g. locally targeted initiatives), and may also reflect illicit drug use that is more detectable. Offence data can, however, offer an insight into the type of offences taking place locally and any emerging trends in substances in use.
Between April 2021 and March 2022, 44% of offences for possession of a controlled drug among over 25s in Blackpool were for cannabis, whilst 26% were for cocaine and 10% for heroin. This compares to 55% cannabis, 22% cocaine and 7% heroin across the wider Lancashire Constabulary area for the same period. 44% of all recorded drug offences in Blackpool were for possession (43% across Lancashire).
For possession with intent to supply offences, 26% involved cannabis, 25% heroin, 22% cocaine and 14% crack. Across Lancashire 29% of possession with intent to supply offences involved cocaine, 28% cannabis, 25% heroin and 9% crack. 20% of all recorded drug offences across both Blackpool and Lancashire were for possession with intent to supply.
Supplying, or offering to supply, a controlled substance comprised 23% of all drug offences in Blackpool during 2021/22, compared to 14% across Lancashire. 77% of these offences involved heroin, 28% crack and 21% cocaine. Across Lancashire 33% of supply offences involved cocaine, 29% heroin, 10% crack and 9% cannabis.
13% of drug offences in Blackpool during 2021/22 involved the production of, or being involved in production of, cannabis.
Drug Related Harm: Drug Deaths
Drug misuse is a significant cause of premature mortality in the UK, and drug related deaths in England and Wales have been on an upward trend over the past decade. This is driven primarily by deaths involving opiates, though also from increases in deaths involving other substances such as cocaine.
Deaths from drug misuse are recorded where a drug controlled under the Misuse of Drugs Act 1971 was mentioned on the death certificate and the cause of death is related to poisoning by drugs, assault by drugs or mental disorders related to volatile substances.
In 2022, 4,572 deaths relating to drug poisoning were registered in England (8.1 deaths per 100,000 population), a 0.9% increase on 2021 figures. Almost two-thirds 64% (2,906) of these deaths were related to drug misuse (5.2 per 100,000). The male drug poisoning death rate of 11.2 is over twice the female rate of 5.2 (both per 100,000).
Almost half (46.1%, 2,261 deaths) of all drug poisoning deaths in England and Wales involved an opiate, though deaths involving cocaine have also risen significantly over the last 10 years (857 deaths in 2022 compared to 139 in 2012). The number of deaths involving methadone (a drug used in opioid substitution treatment) also increased from 367 in 2017 to 640 in 2022.
Polydrug use combinations are a concern: there has been an increasing number of deaths involving benzodiazepines, pregabalin, gabapentin and zopiclone, with 94.6% of these deaths mentioning other drugs, some of them prescribed medication. These drugs are often taken alongside other substances (particularly opiates) and increase the risk of overdose. Pregablin, for example, can be prescribed but can also by obtained illicitly, and can lower the tolerance to heroin. Risk of misuse should be considered when prescribing through primary care.
The increase in deaths involving opiates is set against a decreasing number of new heroin and morphine users. Possible explanations of this include:
-
an ageing cohort of people who use opiates, having increasing co-morbidities / poor general health and being more susceptible to fatal overdose
-
new trends in polydrug use alongside heroin or morphine increasing overdose risk (gabapentinoids and benzodiazepines)
-
disengagement or non-compliance with opiate substitute therapy6
Blackpool has the highest rate of deaths from drug misuse in the country, with 77 deaths between 2020 and 2022 at a rate of 19.5 per 100,000 population (directly standardised rate). The overall rate for England is 5.2 deaths per 100,000 (figure 2). Whilst national and regional rates increased for the COVID-19 affected three-year period 2019-2021, Blackpool's rate fell from 21.3 per 100,000 in the 2018-2020 period to 18.6 in 2019-2021. This was due to the number of deaths to drug misuse reducing from 28 or 29 each year between 2018 and 2020, to 18 in 2021.
Figure 2: deaths from drug misuse, Blackpool, North West and England, 2001-03 to 2020-22 (rate per 100,000 population)
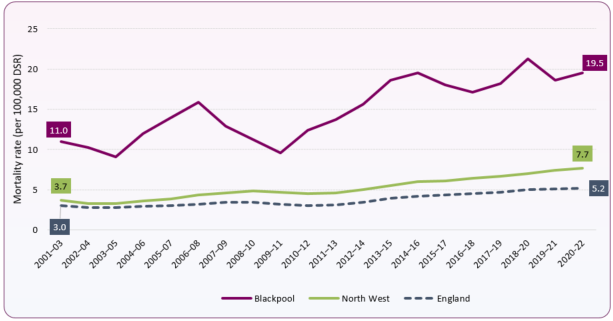 Source: Office for National Statistics (ONS) Deaths related to drug poisoning in England and Wales: 2022 registrations / OHID Public Health Profiles. Missing values indicate numbers too low for disclosure / calculation.
Source: Office for National Statistics (ONS) Deaths related to drug poisoning in England and Wales: 2022 registrations / OHID Public Health Profiles. Missing values indicate numbers too low for disclosure / calculation.
In Blackpool the rate of drug-misuse deaths for men in 2020-2022 was 28.4 per 100,000, the highest in the country. The female rate of 10.8 per 100,000 is the third highest in the country. Both male and female rates have more than doubled since 2009-11 (figure 3).
Figure 3: deaths from drug misuse, Blackpool males and females, 2001-03 to 2020-22 (rate per 100,000 population)
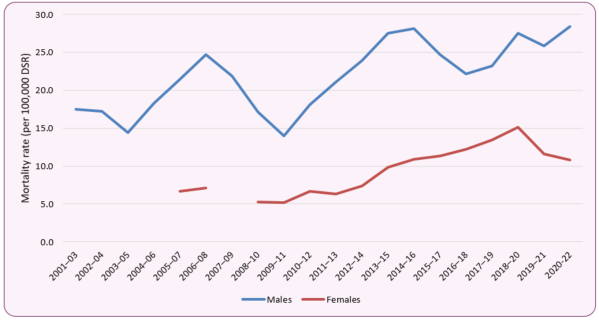 Source: Office for National Statistics (ONS) Deaths related to drug poisoning in England and Wales: 2022 registrations / OHID Public Health Profiles. Missing values indicate numbers too low for disclosure / calculation.
Source: Office for National Statistics (ONS) Deaths related to drug poisoning in England and Wales: 2022 registrations / OHID Public Health Profiles. Missing values indicate numbers too low for disclosure / calculation.
Drug Related Harms: Hospital Admissions7
NHS Digital reports data for drug-related hospital admissions in three main areas:
Admissions for drug-related mental and behavioural disorders
In 2019-20 there were approximately 35 hospital admissions in Blackpool where the primary reason for admission was a drug-related mental and behavioural disorder. Blackpool's hospital admission rate was 30 admissions per 100,000, compared to an England rate of 12.5 per 100,000. This was the 9th highest rate among Local Authorities in England. 2018-19 and 2019-20 rates were the lowest for seven years, and half the 2017-18 rate of 61 admissions per 100,000 population (80 people).
Admissions where drug-related mental and behavioural disorders were a factor in treatment
In addition to the primary reason for admission (above), hospitals collect secondary diagnosis information, where a drug-related mental and behavioural disorder was not necessarily the main reason why a patient was admitted to hospital, but was relevant to the patient's care. In Blackpool during 2019-20 there were 720 hospital admissions where drug-related mental and behavioural disorders were either the primary reason for admission or were a factor in treatment / care. This equates to a crude rate of 569 admissions per 100,000 population, compared to 180.5 per 100,000 across England. The Blackpool rate is the second highest in the country and has been rising steadily since 2015-16.
Admissions for poisoning by drug misuse
In Blackpool during 2019-20 there were 90 hospital admissions for intentional and unintentional poisoning involving a substance listed as being controlled under the Misuse of Drugs Act 1971. The rate of 69 admissions per 100,000 population is the eighth highest in the country and over twice the England average of 31 per 100,000 (Figure 6). Admissions for poisoning by drug misuse in Blackpool have declined since 2015-16 when there were 161 admissions (a rate of 116 per 100,000 population).
Hospital admissions trends can be affected by a range of complex factors, particularly during the COVID-19 pandemic, when hospital presentations and admissions changed significantly. Changes to coding, and protocols for treatment and admission can also affect these statistics, and further exploration of the data is required in order to fully understand the drug misuse admission patterns described above.
Drug Related Harms: Morbidity and Risk Groups
Drug misuse can lead to a range of wider health consequences, with some groups at greater risk.
Blood Borne Viruses, Infection and Injecting Drug Use
Injecting is one of the main causes of health damage related to drug use. People who inject drugs (PWID) are at higher risk of fatal and non-fatal overdose, and the sharing of injecting equipment for drug use is an important contributor to blood-borne virus transmission, including HIV, Hepatitis B and Hepatitis C. People who inject drugs are the group most affected by Hepatitis C in the UK, with over 90% of infections diagnosed in England thought to be acquired through injecting drug use8.
PWID are also vulnerable to a wide range of bacterial infections, as well as other damage to veins and arteries.
The Unlinked Anonymous Monitoring (UAM) Survey of HIV and Hepatitis in People Who Inject Drugs presents annual data across England, Wales and Northern Ireland from PWID who are in contact with specialist services. In 2019, 93% of PWID reported injecting heroin, whilst 57% reported injection of crack cocaine. 20% of respondents reported sharing needles and syringes (the highest proportion since 2010 and an increase from 14% in 2012). 38% of those who injected drugs within the last year reported symptoms of infection at injection sites, with 59% of those not seeking health care treatment.
The 2021 UK Health Security Agency report 'Shooting Up' found that, in 20208:
- 60% of participants in the Unlinked Anonymous Monitoring Survey of HIV and Hepatitis in PWID across England Wales and Northern Ireland had antibodies to Hepatitis C Virus (HCV), an increase of 17% since 2011.
- 20% of PWID in the last year had chronic HCV, a decrease from 33% in 2016 when chronic infection levels were at their highest. This reduction is likely to be due to an increased uptake of direct acting antiviral treatment rather than a reduction in incidence of new infection.
- UAM Survey data suggests that the proportion of PWID infected with Hepatitis B Virus (HBV) has declined from 15% in 2011 to 9.5% in 2019 (2020 data not available due to small sample size).
- HBV vaccination has plateaued in recent years to 66% in 2020, with uptake particularly low among PWID and recent initiates to injecting
- 1.1% of people surveyed who inject psychoactive drugs in England, Wales and Northern Ireland were living with HIV, a lower proportion than many other European countries.
- There were 59 new HIV diagnoses acquired through injecting drug use across England, Wales and Northern Ireland. 38% of these were late diagnoses, where the infection has already started to damage the immune system. One-year mortality among people who acquired HIV through injecting drug use diagnosed late in 2019 was 63 per 1,000, twice as high as the overall late diagnosis one-year mortality rate.
- Opportunities for both Hepatitis B vaccination and HIV testing and treatment continue to be missed.
- Serious bacterial infections in PWID increased in the UK between 2013 and 2019, with a reduction in 2020 corresponding to a period of decreased hospital activity at the height of the Covid-19 pandemic.
- There were 106 reported cases of Invasive Group A streptococcal infection (iGAS) with injecting drug use as a risk factor, less than half the number in 2019 (234).
- There were 35 Meticillin-sensitive and 319 Meticillin-resistant Staphylococcus Aureus (MRSA and MSSA) infections with injecting drug use as a factor in England, compared to 50 and 459 respectively in 2019.
- The potential for cases and outbreaks of illnesses caused by toxins produced by spore-forming bacteria, such as botulism, continues to be a concern, though there were no cases of wound botulism in PWID in the UK in 2020 (there were 7 in 2019) and no cases of clinically confirmed tetanus or anthrax with a history of recent drug injection.
In 2020-21, 20% of all new presentations to the specialist drug treatment service in Blackpool were currently injecting drugs, with a further 26% having previously injected. The vast majority of injecting users were receiving treatment for opiate use, and 32.3% of new opiate presentations to the service were currently injecting drugs.
Nationally, there are concerns that the COVID-19 lockdown period has been a contributory factor in increases in risk behaviours (particularly the sharing of injecting equipment). COVID-19 has had a significant impact on PWID and service provision, and it will be important to monitor any continued impact on the drug user population.
Co-occurring Mental Health and Drug Use Conditions
Mental health problems are experienced by around 70% of drug users in community substance misuse treatment, with death by suicide also common. Those with co-occurring mental health and drug misuse issues are at higher risk of relapse (both in terms of substance misuse and mental health), can experience barriers to accessing services, and often have wider health and social needs. Tackling co-occurring severe mental health problems and drug use (sometimes referred to as 'dual diagnosis') can be complex, and requires a strong therapeutic alliance and collaborative delivery of care between drug treatment and mental health services9,10.
Data from the National Drug Treatment Monitoring System suggested that 23.5% of new presentations to the drug treatment service in Blackpool during 2016-17 had concurrent contact with mental health services. This was similar to the national level of 24.3%. In 2020-21 the treatment services identified that 63% of those entering drug treatment in Blackpool were identified as having mental health treatment needs, the same proportion as in England. The proportion was higher in female new presentations (69% in Blackpool compared to 73% in England).
Parental Drug Use
Parental substance misuse is a significant public health concern. The 2003 'Hidden Harm' report by the Advisory Council on the Misuse of Drugs (ACMD) estimated that there were between 200,000 and 300,000 children in England and Wales where one or both parents had serious drug problems. Parental drug misuse can compromise children's health and development from conception onwards, though the risks of harm may be reduced through treatment and support for the affected adult, and by the presence of at least one other consistent parent or carer, a stable home with adequate finances, maintenance of family routines and activities, and regular attendance at a supportive school11.
Based on data from the National Drug Treatment Monitoring Service (NDTMS), there were an estimated 514 opiate dependent adults living in Blackpool with children in 2014-15, at a rate of 6 per 1,000 population.
In 2021 19.9% (560) of all Blackpool's Children in Need assessment episodes identified drug misuse by the parent as a factor. Nationally, 15.5% of assessments identified parental drug misuse as a factor in Children in Need episodes.
22.4% of the 1,250 people in drug treatment in Blackpool in 2020-21 were living with children. There were approximately 220 parents who were living with their own children, with around 185 of those receiving treatment for opiate use. A further 310 of those in treatment were parents who were not living with their children (245 opiate users), and 60 (55 opiate users) were not a parent but were living in a property with children present. The proportion of opiate users in treatment who were living with children is similar to national levels (Figure 7).
Source: NDTMS. Note: NDTMS numerical data is rounded to the nearest 5 to prevent patient identification. Proportions are rounded to nearest whole percentage point, and as a result may not total 100%
In addition to parental drug use, parental alcohol misuse is also a concern - see Alcohol section for further information.
Drug Treatment
Specialist drug and alcohol treatment services for adults (and young people) are commissioned by the Local Authority. In Blackpool adult services are provided by 'Horizon', a partnership between Delphi Medical and Acorn Recovery Projects, together with Renaissance UK and Blackpool Council. Services for children and young adults under 25 are provided by Blackpool Adolescent Service. Information about drug and alcohol treatment services is compiled nationally through the National Drug Treatment Monitoring System (NDTMS).
People in Treatment12
In Blackpool in 2020-21 there were around 1,250 people in drug treatment. Of these 1,010 (81%) were in treatment for opiate use, 125 (10%) for non-opiate use only, and 115 (9%) for a combination of non-opiate use and alcohol. Overall numbers in treatment in Blackpool have remained relatively steady since 2014-15, having fallen by 34% over the first half of the 2010s decade. This was primarily due to a reduction in people in treatment for opiate use between 2009-10 and 2014-15 (Figure 8). A similar trend was seen nationally over this period, though the reduction was around 11%.
Figure 8: Numbers in Drug Treatment by Substance Type, Blackpool 2009/10 to 2020/21
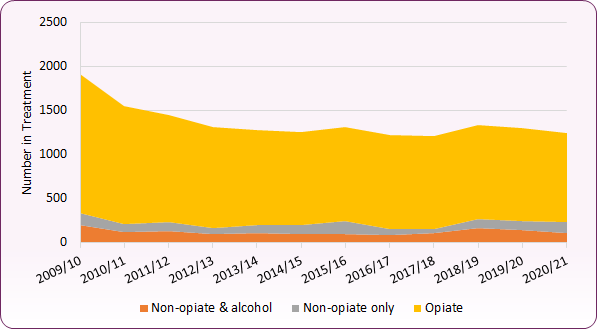 Source: NDTMS
Source: NDTMS
Blackpool has around 2 1/2 times the rate of people in drug treatment than the national average. In 2020/21 the crude rate of those in drug treatment (excluding treatment for alcohol only) was 1,142 per 100,000 adult population, compared to 448 per 100,000 nationally. The crude rate of those in treatment for opiate use was 924 per 100,000, almost three times the England rate of 317 per 100,000.
Two-thirds (66.7%) of those in drug treatment are male, compared to 71.4% nationally. Blackpool has a higher proportion of female opiate users within treatment (33.1%) than the national average (27.6%). These proportions have remained relatively stable over the past ten years.
99.4% of those in treatment identified their ethnicity as White (96.7% of the Blackpool population was estimated to be White in the 2011 census).
67% of those in drug treatment are aged between 30 and 49 years. Whilst the overall number of 18 to 49 year olds in treatment has been reducing, the number of those aged over 50 increased from 80 in 2009-10 to 260 in 2020-21, and over 50s now account for 20.7% of the Blackpool treatment population (Figure 9). This increase is primarily due to an ageing opiate user population across the country, with the number of opiate users aged 50+ in treatment in Blackpool increasing from 60 in 2009-10 to 240 in 2020-21. The ageing opiate user cohort tend to have more complex needs due to deteriorating physical and mental health, difficulties navigating health and care systems, and stigma associated with substance use13.
Figure 9: Numbers in Drug Treatment by Age Group, Blackpool 2009/10 to 2020/21
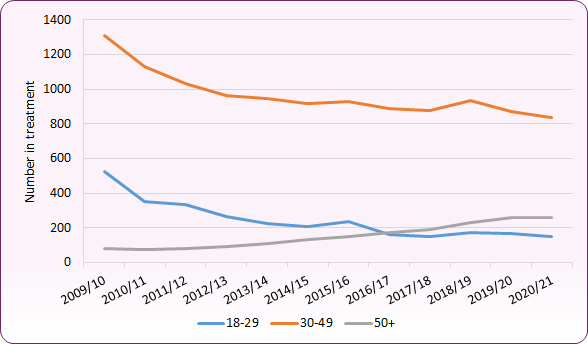 Source: NDTMS
Source: NDTMS
In contrast, 59% (n=75) of non-opiate only users (non opiate users without alcohol concerns) in treatment were aged between 18 and 29 years, compared to 46% nationally (Figure 10).
Source: NDTMS
The majority (58%) of those in drug treatment have been in treatment for less than two years. 28% (350 people) have been in treatment for four or more years (nationally 26%). All of these are opiate users, highlighting the complex nature of opiate treatment and recovery for many people. The number of those in long-term (4+ years) treatment in Blackpool rose from 280 in 2014-15 to 360 in 2019-20.
New Presentations
A new presentation to drug treatment services is defined as when a person starts a new treatment journey, either for the first time or returning to treatment having had a break of over 21 days. Information about new presentations to drug services can help to gain insights into current issues and trends relating to drug use and the needs of people who use drugs.
In 2020-21 there were 430 new presentations to the specialist service in Blackpool for drug-related problems. This is an 18% reduction from pre-COVID 2019-20. New presentations for opiate use dropped 25%, non-opiate and alcohol presentations fell by 18%, whilst non-opiate only presentations increased by 14%. A similar trend is observed nationally, and may reflect changes to drug use, supply and access to services over the coronavirus lockdown period. Overall, however, 61.9% of new presentations were for opiate use compared to 47.8% nationally during this period.
68% of all new presentations to the service reported opiate and / or crack use, with 40% reporting both. 30% of all new presentations reported cannabis use, 26% alcohol use, 13% cocaine use and 10% use of benzodiazepines (14% of opiate users).
Figure 11: New Presentations to Specialist Drug Service by Drug Type, Blackpool 2009/10 to 2020/21
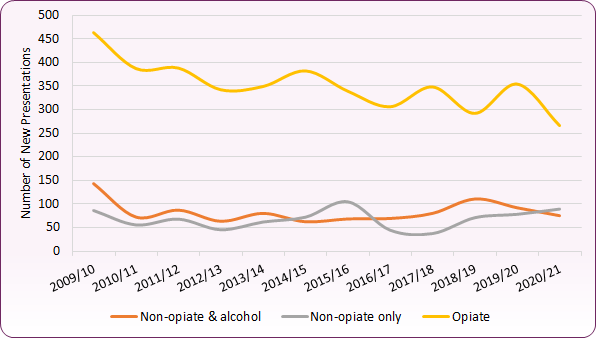 Source: NDTMS
Source: NDTMS
As with the overall treatment population, around two-thirds (67.7%) of new presentations were male. 67.5% were among those aged 30 to 49 years, 22.4% among those aged 18 to 29 years, and 10.2% among 50s and over. 78% of those presenting in the 50+ age group were male.
23% of all new presentations reported a housing problem, with 5.1% reporting an urgent problem. Among opiate users 29.6% reported a housing problem, with 7.9% reporting an urgent problem. This is similar to national levels of reported housing need for the treatment population, though the proportion reporting urgent need is lower in Blackpool.
Two thirds (66.6%) of those presenting to the specialist drug service in 2020-21 were unemployed or economically inactive, whilst 19.9% were registered as long-term sick or disabled. Only 12.5% of new presentations were in regular employment, compared to 22.4% of new presentations nationally.
59.8% of referrals to the specialist drug service in 2020-21 were self-referrals or came from family and friends. In 2019-20 the proportion was 69.5%, and there were over 100 fewer self-referrals during the 2020-21 COVID-19 affected period. Referrals from criminal justice (16.9%) and health and social care (6.3%) also reduced in 2020-21, though referrals from other sources (18.8%) almost trebled.
Treatment Outcomes
The OHID Public Health Outcomes Framework measures a 'successful completion' of treatment as those adults successfully completing and not re-presenting within 6 months as a proportion of the overall number in treatment for that type of substance.
For opiate users, the percentage of successful completions has been reducing since 2013 (Figure 12). Blackpool's completion percentage of 3.8% in 2020 remains lower than the national average of 4.7%. A steeper decline in 2020 may be due to the impact of COVID-19 on services and treatment14.
Figure 12: Successful Completion of Drug Treatment: Opiate Users, Blackpool and England 2010-20
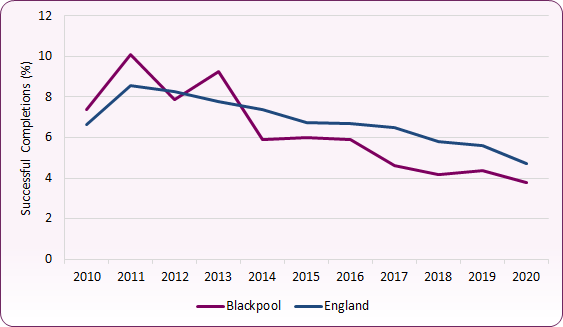 Source: OHID Public Health Outcomes / NDTMS
Source: OHID Public Health Outcomes / NDTMS
For non-opiate users the percentage of successful completions is significantly higher, in part due to the differences in treatment length between opiate and non-opiate users. In Blackpool in 2020 30% of non-opiate users successfully completed treatment, compared to 33% across England. Blackpool's non-opiate completion percentage fell sharply between 2016 and 2018, before improving in 2019 and 2020 (Figure 13).
Figure 13: Successful Completion of Drug Treatment: Non-Opiate Users, Blackpool and England 2010-20
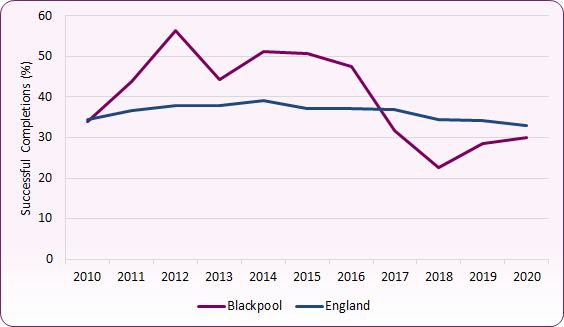 Source: OHID Public Health Outcomes / NDTMS
Source: OHID Public Health Outcomes / NDTMS
In 2020-21, 330 people exited the specialist drug service in Blackpool. Of those, 36.6% successfully completed treatment, compared to 42.2% nationally. This proportion varies by type of substance, with 23.2% of opiate users exiting the services successfully completing treatment (24.7% nationally) compared to 56% of non-opiate users (57% nationally), and 50.7% of non-opiate users with alcohol use (54.6% nationally).
31.1% of those exiting the service dropped out of treatment (compared to 35.4% nationally), 17.8% transferred to another service inside or outside custody (compared to 15.1% nationally). 8.8% of treatment 'exits' died (compared to 4.1% nationally).
Nationally, the proportion of deaths among the total treatment population (including alcohol) increased from 1.1% to 1.4%, the largest increase since data collection commenced. 2% of Blackpool's drug treatment population (including alcohol) died in 2020-21 (2.3% of the drug treatment population excluding those in treatment for alcohol only). This was a similar level to 2019-20 but an increase from 1.2% in 2015-16.
National and Local Strategy and Response
Following phase two of Dame Carol Black's review of drugs in 2021, the UK Government released From Harm to Hope: A 10-year drugs plan to cut crime and save lives. The plan focuses on three strategic priorities:
- Breaking supply chains - focused on preventing drug supply and disrupting gang operations
- Delivering a world-class treatment and recovery system - rebuilding local authorities treatment and recovery services, ensuring service integration, improving access, developing the workforce and improving criminal justice pathways
- Achieving a generational shift in demand for drugs - changing attitudes in society around the acceptability of drug use, applying tougher consequences and delivering prevention and early intervention.
By 2024-25 the UK Government aims to prevent nearly 1,000 deaths and provide at least 54,500 new treatment places, as well as targets to prevent crimes, disrupt organised crime activity and seize criminal assets.
Since the release of the strategy the Government has issued further guidance for local delivery partners, including the publication of a National Combating Drugs Outcome Framework and the establishment of local Combating Drugs Partnerships. The Combating Drugs Partnership will comprise of a range of local partners (including the Local Authority, Police, Probation Service and Integrated Care Board) and will be accountable for delivery against the National Combating Drugs Outcome Framework. In Blackpool, plans are in place to establish a Combating Drugs Partnership in 2022.
As an area with high levels of drug misuse and drug-related harm, Blackpool has been a pathfinder site for Project ADDER since 2021. Project ADDER is a joint Home Office and Department for Health and Social Care programme seeking to:
- reduce drug-related death
- reduce drug-related offending
- reduce the prevalence of drug use
- deliver sustained and major disruption of high-harm criminals and networks involved in middle market drug / firearms supply and importation
In addition to this, the Blackpool Drug Harm Reduction Strategy 2020-22 sets out Blackpool's strategy to reduce the number of people who suffer harm, directly or indirectly, because of the prevalence of drug misuse in the town.
As part of the Strategy’s response to drug related deaths and non-fatal overdoses, an integrated real time surveillance programme has been introduced across Blackpool. Blackpool Council, Lancashire Constabulary, Horizon Drug Treatment Service and other partners work together to rapidly record and report drug related deaths and non-fatal overdoses, examining contributory factors that might prevent further harms. Lancashire Constabulary have also initiated a drug testing protocol whereby any substances seized at the site of suspected drug related deaths or non-fatal overdoses can be tested for information purposes. Information is shared via Project ADDER to aid response and prevention activity, and any alerts relating to substances of concern are circulated via a Lancashire-wide Local Drugs Information System (LDIS) network.
Naloxone is an opioid antagonist that can be used to reverse the effects of opioids such as heroin, methadone, codeine, morphine, opium and buprenorphine. It can potentially save someone's life in the event of an overdose, though effects don't last very long and medical help is still necessary. Naloxone is used by medical practitioners (including the NW Ambulance Service) and is also available to drug users via the Delphi drug treatment service, Renaissance and Lived Experience. A pilot is commencing in September 2022 to enable police connected to Project ADDER to carry naloxone with a view to extending it to the wider force in future.
[] Black, Dame C. (2020) Review of Drugs - evidence relating to drug use, supply and effects, including current trends and future risks. Home Office, February 2020.
[] Office for National Statistics (ONS) Drug misuse in England and Wales: year ending March 2020.
[] The ‘any drug’ / overall use category consists of amphetamines, anabolic steroids, cannabis, powder cocaine, crack cocaine, ecstasy, heroin, ketamine, LSD, magic mushrooms, mephedrone, methadone, methamphetamine, tranquillisers, unknown pills or powders, something unknown smoked and any other drug. Class A drug use includes powder cocaine, crack cocaine, ecstasy, heroin, LSD, magic mushrooms, methadone and methamphetamine
[] Offce for Health Improvement and Disparities and UK Health Security Agency. Estimates of the prevalence of opiate use and / or crack cocaine use. GOV.UK, October, 2023
[] Aldridge, J., Garius, L., Spicer, J., Harris, M., Moore, K. & Eastwood, N. (2021) Drugs in the Time of COVID: The UK Drug Market Response to Lockdown Restrictions, London: Release.
[] Office for National Statistics (ONS) Deaths related to drug poisoning in England and Wales: 2020 registrations. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2020
[] These statistics are set in a context of overall increasing emergency admissions within Blackpool Teaching Hospitals NHS Trust. Between 2013/14 and 2018/19 total emergency admissions for all conditions / diagnoses increased by 29%, levelling off in 2019/20.
[] UK Health Security Agency (UKHSA) (2021) Shooting Up: infections and other injecting-related harms among people who inject drugs in the UK, 2020, update December 2021 and Shooting Up: data tables accompanying the report, update December 2021.
[] Public Health England (PHE) (2017) Better care for people with co-occurring mental health and alcohol / drug use conditions.
[] National Institute for Health and Care Excellence (NICE) (2016) Coexisting severe mental illness and substance misuse: community health and social care services. NICE Guidance [NG58].
[] Advisory Council on the Misuse of Drugs (ACMD) (2003) Hidden Harm - responding to the needs of children of problem drug users.
[] NDTMS records treatment across four categories for all those aged over 18: opiate, non-opiate, non-opiate and alcohol, and alcohol only. 'Alcohol only' treatment is excluded in this report (see Alcohol JSNA section for further information about alcohol treatment).
[] Advisory Council on the Misuse of Drugs (ACMD) (2019) ACMD report - Ageing cohort of drug users, June 2019.
[] Office for Health Improvement and Disparities (OHID) Adult substance misuse treatment statistics 2020 to 2021: report.