Sexual Health
Last Modified 28/02/2024 12:24:16
Share this page
Introduction
Sexual health is an important and integral part of overall health. This is captured in the working definition of sexual health developed by the World Health Organisation (WHO):
‘Sexual health is a state of physical, emotional, mental and social wellbeing in relation to sexuality; it is not merely the absence of disease, dysfunction or infirmity. Sexual health requires a positive and respectful approach to sexuality and sexual relationships, as well as the possibility of having pleasurable and safe sexual experiences, free of coercion, discrimination and violence. For sexual health to be attained and maintained, the sexual rights of all persons must be protected, respected and fulfilled’1
The local authority has a mandated responsibility to commission comprehensive, open access sexual and reproductive health services. Free and confidential open access services are essential to control infection, prevent outbreaks and reduce unwanted pregnancies and non-residents are entitled to use the sexual health services provided in Blackpool.
Sexual ill health is not equally distributed among the population. Those at highest risk of poor sexual health are often from specific population groups with varying needs. These groups include; young people, men who have sex with men (MSM), people from African communities, people living with the human immunodeficiency virus (HIV), sex workers, victims of trafficking, victims of sexual and domestic violence and abuse and other marginalised or vulnerable groups.
Condomless sex, particularly with new or casual partners, is a major driving force behind STI infection, and the use of condoms remains the primary way of reducing the risk of picking up or passing on an infection, as well as reducing the risk of unintended pregnancy. Regular testing for HIV and STIs is also important to maintaining good sexual health, and it is recommended that everyone having condomless sex with new or casual partners should be screened for STIs and HIV on an annual basis. Men who have sex with men should screen on an annual basis and at three month intervals if having condomless sex with new or casual partners. Women aged under 25 should also be screened for chlamydia on changing sexual partner and on an annual basis.
People at risk of HIV can also use HIV pre-exposure prophylaxis (PrEP) to reduce the risk of establishing a permanent infection if exposed to the virus during sex.
The Blackpool Sexual Health Needs Assessment was completed in 2022 and the Sexual Health Strategy 2023-2026 has been designed to deliver on our vision to support everyone to achieve optimal sexual health and wellbeing, regardless of their circumstances, and to be able to access the sexual health services that they need, when they need them.
The strategy builds on the progress made by the previous 2017-2020 sexual health strategy and on the findings of the 2022 sexual health needs assessment for Blackpool. The strategy provides a strategic framework to shape the planning and delivery of services and interventions to enable the vision to be realised.
Facts and figures
For the most recent Summary Profile of Local Authority Sexual Health for Blackpool, published by the Office for Health Improvement & Disparities, please click here.
Testing and partner notification are essential elements of STI management and control, protecting patients/partners from re-infection and long-term consequences from untreated infection, reducing the cost of complications and onward transmission.
In 2019, there were 467,096 new STI diagnoses made at Sexual Health Clinics in England (a rate of 830 per 100,000 population). Of these, the most commonly diagnosed STIs were chlamydia (49%), gonorrhoea (15%), genital warts (11%), and genital herpes (7%).
In COVID-19 affected 2020, there were 317,901 new STI diagnoses in England (a rate of 562 per 100,000). This represents an overall 32% decrease from the previous year, with drops in new diagnoses of chlamydia (-29%), gonorrhoea (-20%), syphilis (-14%), genital warts (-46%) and genital herpes (-40%). These reductions reflect fewer examinations and tests carried out during 2020, with the largest drops observed in those STIs that tend to be diagnosed by physical examination.
COVID-19 has impacted on sexual health and sexual health services in a numbers of ways. Data from the National Survey of Sexual Attitudes and Lifestyles (NATSAL) COVID study suggests that fewer people met new sexual partners in 2020, and the number of sexual partners met reportedly reduced. However, a substantial proportion of people still had ongoing risk for STIs / HIV, and two thirds of those who reported having a new sexual partner during this period also reported not using a condom. COVID-19 resulted in the overall number of sexual health service consultations reducing by 10% nationally in 2020, and the number of full STI screens reduced by 25% over this period2. Sexual health services both nationally and locally made significant adaptations to their services, with the introduction or expansion of online services (including testing) and remote consultations accompanying face-to-face consultation for those in urgent need. Because of lockdowns and the adaptations mentioned, the data presented here reports primarily on 2019, though trend data showing service impact in 2020 is also shown.
There were 1,547 new STIs diagnosed in residents of Blackpool in 2019, a rate of 1,109 per 100,000 residents (compared to 830 per 100,000 in England). Blackpool was ranked 24th highest for all new STI diagnoses out of 149 upper tier local authorities. In COVID-19 affected 2020, there were 944 new STIs diagnosed, a rate of 682 per 100,000 residents (compared to 562 per 100,000 in England).
Overall, diagnoses of new STIs remained relatively steady in Blackpool between 2016 (1,525 new diagnoses) and 2019 (1,547) following a reduction from 2012 (2,038) to 2016.
Figure 1: New STI diagnoses in Blackpool, 2019
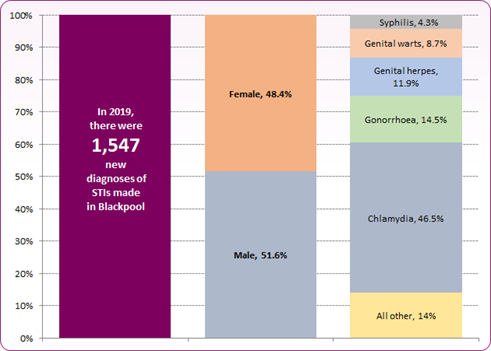 Source: PHE Sexual and Reproductive Health Profiles and PHE GUMCADv2 Report
Source: PHE Sexual and Reproductive Health Profiles and PHE GUMCADv2 Report
However, when looking at new STI diagnoses excluding young people aged under 25 (the age group targeted by the National Chlamydia Screening Programme (NCSP)), the number and rate has risen from 2014 to 2019 (with the exception of 2017) (figure 2). The trend in new STI diagnoses (exc. Chlamydia <25) in Blackpool remains significantly higher than the national average.
Figure 2: Trend in new STI diagnosis rate per 100,000, Blackpool compared to England
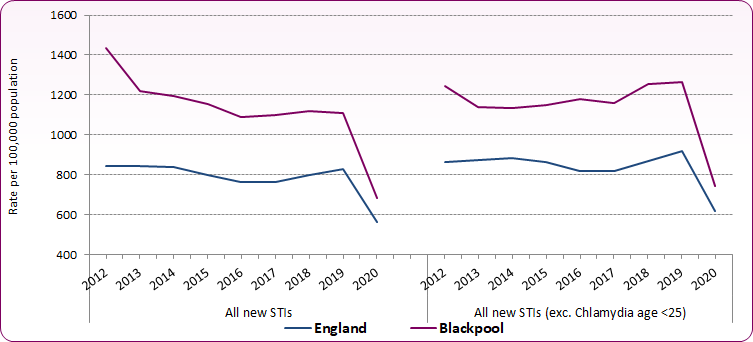 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
The five main STI diagnoses in Blackpool are chlamydia (46.5% of all new diagnoses), syphilis (4.3%), gonorrhoea (14.5%), genital herpes (11.9%) and genital warts (8.7%). Other STIs account for the other 14% of infections. Of the five main STIs diagnosed, 97% of females are in the heterosexual population. For males, 67% identified as heterosexual while 30% are gay or bisexual.
Figure 3 shows the trend in specific STI infection rates since 2012.
Increases in gonorrhoea reflect a national picture which has seen a sharp rise in recent years, exceeding 70,000 cases across England in 2019. Between 2016 and 2018 Blackpool diagnoses increased more sharply than the national average, though 2019 figures saw the rate levelling off at 161 per 100,000 of the population (compared to the national rate of 126 per 100,000). Although improved test sensitivity and uptake may have contributed, increased gonorrhoea transmission is likely playing a major role. Reversing this trend is a public health priority given the spread of resistance to frontline antimicrobials used for treating gonorrhoea and the depletion of effective treatment options. The UK's five year action plan (2019-2024) for tackling antimicrobial resistance and the Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) Protocol seek to tackle this, with updated PHE guidance for the detection of gonorrhoea in England (2021) making recommendations on effective testing regimes and care pathways.
New diagnoses for syphilis in England gradually rose between 2000 and 2012, before increasing rapidly from 2013 to 2019 (3,337 to 8,011 new diagnoses). In Blackpool, following a downward trend between 2013 and 2016, the number and rate of new syphilis diagnoses also increased rapidly from 2016 to 2019, with a sharp rise (almost double the number of diagnoses) in 2019. The PHE Syphilis Action Plan (2019) emphasises the need to strengthen public health measures and reduce transmission of syphilis, recommending a range of testing, partner notification, antenatal screening and health promotion measures intended to increase awareness, improve detection and reduce transmission of the disease.
Syphilis and gonorrhoea infections are predominantly concentrated in core risk groups, particularly in men who have sex with men (48% of all new gonorrhoea and 69% of new syphilis diagnoses in England in 2019). However, national increases have also been seen in the number of diagnoses among heterosexuals and in the number of cases of congenital syphilis since 20113.
There has been a general fall in genital wart infection and this is expected to continue as a positive effect from the national Human Papilloma Virus (HPV) vaccination programme for young women, and for MSM up to the age of 45 years of age (from April 2018).
Whilst rates for new infections of genital herpes have remained relatively steady across England since 2012, new diagnoses in Blackpool rose from a rate of 90 per 100,000 in 2013 to 141 per 100,000 in 2018. The rate did, however, fall back to 132 per 100,000 in 2019. This increase may in part be due to the use of more sensitive tests (NAATs).
Figure 3: Trends by sexually transmitted infection, 2012-2020
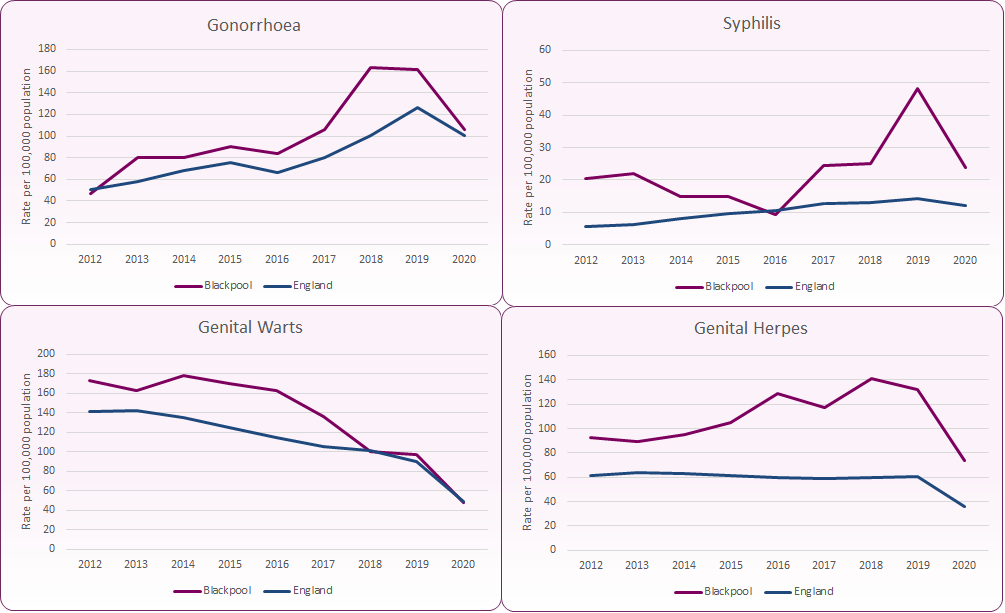 Source: PHE, Sexual and Reproductive Health Profiles
Source: PHE, Sexual and Reproductive Health Profiles
Of the 1,547 new diagnosed STIs in 2019, 48% (742) were in the under 25 age group. Of these 41% were male and 59% female. Conversely, in the 25+ age group, 61% of new diagnoses were male and 39% female. In comparison, across England 47% of new diagnosed STIs were in the under 25 age group and the gender split is broadly the same as Blackpool. For the 25+ age group across England 65% of new diagnoses were in males and 35% in females.
Figure 4: All new STIs in Blackpool by gender and age group, 2019
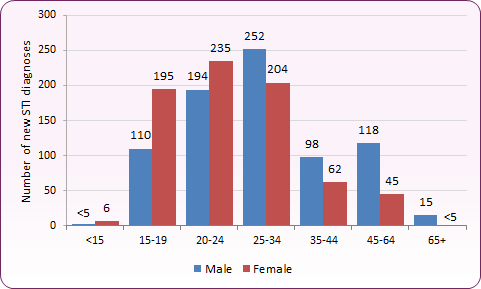 Source: PHE, GUMCADv2 Report, Numbers and Rates of New STIs Diagnoses, HIV and STI Portal
Source: PHE, GUMCADv2 Report, Numbers and Rates of New STIs Diagnoses, HIV and STI Portal
Figure 5 shows the breakdown by STI diagnoses for males by sexual orientation. Variations in identified sexual orientation across different STIs can clearly be seen, with 67% of new syphilis diagnoses being to men identifying as gay, compared to 19% for new chlamydia diagnoses.
Figure 5: Number and proportion of STIs in males by identified sexual orientation, 2019
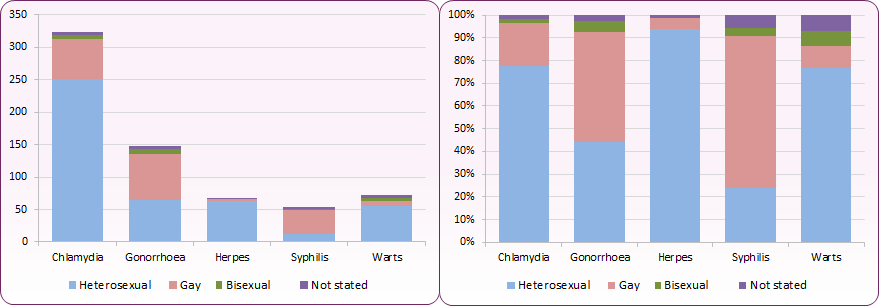 Source: PHE, GUMCADv2 Report, Numbers and Rates of New STIs Diagnoses, HIV and STI Portal
Source: PHE, GUMCADv2 Report, Numbers and Rates of New STIs Diagnoses, HIV and STI Portal
For cases in men where sexual orientation was known, 29.9% of new STIs in Blackpool were among gay, bisexual and other MSM, compared to 36.4% in England4.
There is a concern nationally at the rise in syphilis and gonorrhoea among MSM which link with high levels of condomless sex. HIV serosorting, (the practice of engaging in condomless sex with partners believed to be of the same HIV status) increases the risk of infection from STIs, hepatitis B and C, and sexually transmissible enteric infections like Shigella spp, and likely plays a role in the reported STI trends. For those who are HIV negative, serosorting increases the risk of HIV seroconversion, and an estimated 6% of people living with HIV in the UK in 2019 are undiagnosed5.
While vaccination is a measure that can be used to control genital warts and hepatitis B, control of other STIs relies on consistent condom use, behaviour change to decrease overlapping and multiple partners, ensuring good access to testing and treatment, and ensuring partners of cases are notified and tested. The large fall in genital warts in young women is an expected positive effect of the national HPV vaccination programme.
STI testing rates, positivity and diagnoses rates are linked. Figure 6 shows STI diagnosis (HIV, syphilis, gonorrhoea and chlamydia in those aged 25+) positivity among people accessing sexual health services (SHS) expressed as a percentage of the total number of people tested for one or more infections at a new attendance.
Figure 6: STI testing positivity percentage (HIV, Syphilis, Gonorrhoea and Chlamydia aged 25+) - Blackpool, England and North West
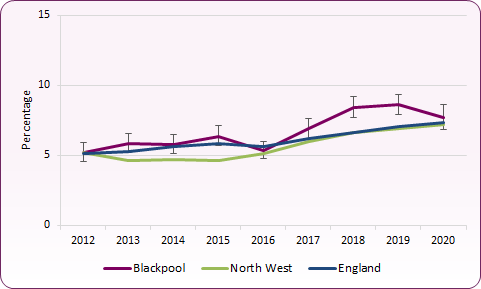 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
In 2019, Blackpool's testing positivity was 8.6%, higher than both the North West (6.9%) and England (7.1%).
Re-infection
Reinfection with an STI is a marker of persistent risky behaviour. In Blackpool, an estimated 8.5% of women and 9.9% of men presenting with a new STI at a GUM clinic during the five year period from 2015 to 2019 became re-infected with a new STI within twelve months. Nationally, during the same period of time, an estimated 7.1% of women and 9.9% of men presenting with a new STI at a GUM clinic became re-infected with a new STI within twelve months4.
Also, an estimated 4.4% of women and 7.5% of men diagnosed with gonorrhoea at a sexual health service (SHS) clinic in Blackpool between 2015 and 2019 were re-infected within twelve months. Nationally, an estimated 4.1% of women and 11.5% of men became re-infected with gonorrhoea within twelve months.
In Blackpool, an estimated 13% of 15-19 year old women and 10.7% of 15-19 year old men presenting with a new STI at a SHS clinic during the five year period from 2015 to 2019 became re-infected with an STI within twelve months. Teenagers may be at risk of reinfection because they lack the skills and confidence to negotiate safer sex.
The NCSP was established in 2003 to facilitate early detection and treatment of asymptomatic Chlamydia infection. Chlamydia is the most common bacterial sexually transmitted infection in England and up to 70% of women and 50% of men with the infection have no symptoms. If these infections remain undiagnosed and hence untreated, complications such as pelvic inflammatory disease, ectopic pregnancy and tubal factor infertility can develop. Effective screening, when combined with good sexual health improvement messages, contributes to young people having better sexual health, as the offer of a test normalises testing for STIs, doesn't increase risky behaviour and provides a gateway to more comprehensive sexual health services.
In November 2017 a review of the programme commenced, resulting in the 2021 announcement of a shift towards reducing the harmful effects of untreated chlamydia infection, which predominantly affect women. This will refocus the programme on opportunistic screening for young women, discontinuing the offer of opportunistic screening to young men outside sexual health services (in settings such as GPs and pharmacies). All young people will still be able to access chlamydia tests at sexual health services and young men will continue to be contacted and tested through partner notification processes.
The Public Health Outcomes Framework (PHOF) includes an indicator to assess progress in controlling chlamydia in sexually active young adults. This currently recommends local areas achieve an annual chlamydia detection rate of at least 2,300 per 100,000 15-24 year old resident population to detect and treat sufficient asymptomatic infections to effect a decrease in incidence. Measures and targets are likely to change as a result of the recent evidence review and the focus on opportunistic screening for young women.
The chlamydia detection rate per 100,000 young people aged 15-24 years in Blackpool was 2,776 (compared to 2,058 per 100,000 in England) in 2019. The rate reflects both screening coverage levels and the proportion of tests that are positive at all testing sites, including primary care, sexual and reproductive health and genitourinary medicine services. Areas achieving or above the 2,300 detection rate should aim to sustain or increase, with areas achieving below it aiming to increase their rate. As shown in figure 7, Blackpool has a higher detection rate than England, though the detection rate has shown a decline. The fall between 2012 and 2013 was due to more targeted screening while the fall from 2014 to 2015 is in line with the national picture, where the rate has fallen by 7.3%. The fall between 2017 and 2019 is in line with a regional decline, but contrasts with a slight increase in the overall English rate.
Figure 7: Chlamydia detection rate per 100,000 aged 15-24
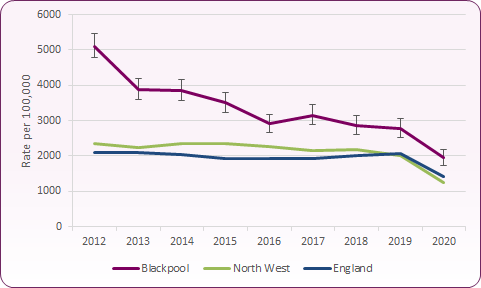 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
Nationally chlamydia detection rates are higher in females than males reflecting higher testing rates in females (figure 8).
Figure 8: Chlamydia detection rate per 100,000, females and males aged 15-24
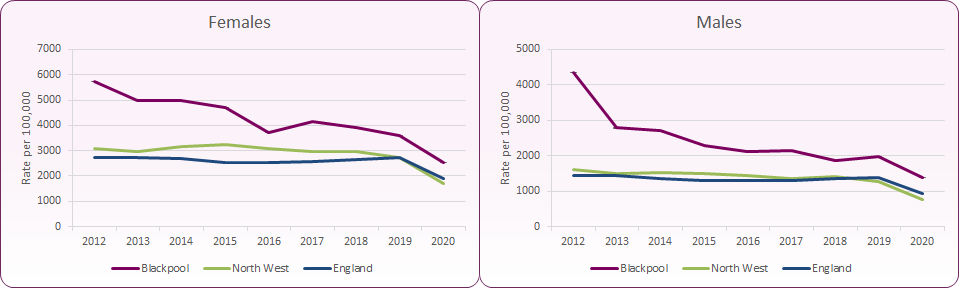 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
Nationally, chlamydia detection rates among young females did not vary greatly between those aged 15-19 years and those aged 20-24 years. However, detection rates among males aged 20-24 years were up to 2.2 times higher than among males aged 15-19 years.
Chlamydia test coverage data represent the number of tests reported, and not the number of people tested. Until the recent review, the NCSP recommended that all sexually active under 25 year old men and women be tested for chlamydia annually or on change of sexual partner (whichever is more frequent). There has been a decline in chlamydia testing coverage nationally and Blackpool has shown a similar decline since 2012, though the proportion tested in Blackpool has been consistently higher than the national average (figure 9). The decline is mostly attributable to fewer tests being carried out in non-specialist sexual health services and community venues. Improvements have also been made in data quality which may also account for the decline in data coverage with a reduction in double counting.
Figure 9: Proportion of 15-24 year olds screened for chlamydia, 2012-2020
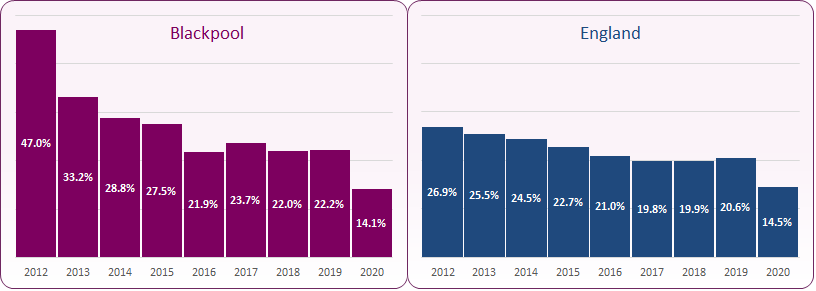 Source: PHE, HIV STI Portal
Source: PHE, HIV STI Portal
The proportion of chlamydia tests that were carried out in males aged 15-24 years in 2019 was 26.6%, compared to 73.4% of females in the same age range (figure 10).
Figure 10: Proportion of Chlamydia tests by age and gender ( under 25 year olds), 2019
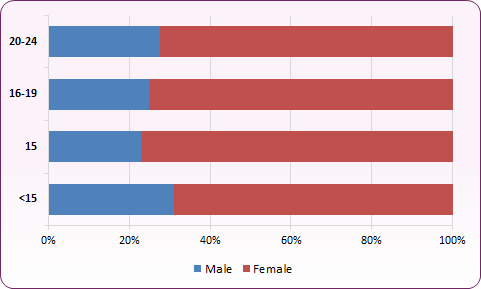 Source: PHE, HIV STI Portal (CTAD / GUMCAD combined data)
Source: PHE, HIV STI Portal (CTAD / GUMCAD combined data)
The NCSP recommends that local authorities commission services that achieve a positivity rate of 5-12%. In 2019, 22.2% of 15-24 year olds were tested for chlamydia with a 12.5% positivity rate. Nationally, 20.6% of 15-24 year olds were tested for chlamydia with a 10% positivity rate.
The majority of Blackpool residents use sexual health services within Blackpool. In 2019, only 2% of Blackpool service users attended clinics outside of Blackpool. However, of all patients using services within Blackpool, 41% come from outside the local authority (Figure 11). Of those, 87% were resident in neighbouring Fylde and Wyre.
Figure 11: Patients attending clinics in Blackpool by residency status, 2019
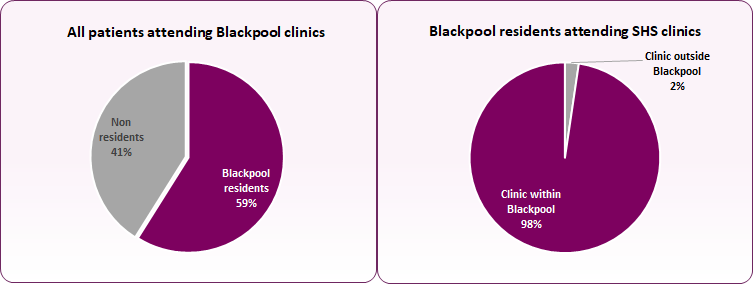 Source: GUM Clinic Activity Dataset report, HIV and STI Web Portal
Source: GUM Clinic Activity Dataset report, HIV and STI Web Portal
Genitourinary Medicine (GUM) clinic
The number of patients accessing the GUM service at Whitegate Drive Health Centre remained relatively steady between 2017 and 2020 (figure 12). 97.8% of Blackpool residents choose to attend the GUM service in Blackpool, making up 56% of patient flow from 2017-2019. The majority of the remaining patients attend from the Fylde and Wyre area. During COVID-19 affected 2020 Whitegate Drive became a hub for telephone and postal testing services for both Blackpool and Lancashire Sexual Health Services, resulting in a lower proportion of Blackpool patients reported as being 'seen' by the clinic during this period.
Figure 12: Attendances to Whitegate Health Centre GUM by Blackpool residents 2011-2020
| | Patients | Attendances |
|---|
| | Patients from Blackpool | % of patients seen by clinic | New attendances | Follow-up attendances | Total attendances |
|---|
| 2020 |
4,584 |
28%* |
7,830 |
1,539 |
9,396 |
| 2019 |
4,894 |
56.4% |
6,837 |
1,323 |
8,160 |
| 2018 |
4,395 |
53.6% |
5,840 |
1,396 |
7,236 |
| 2017 |
4,399 |
55.5% |
5,575 |
2,048 |
7,623 |
| 2016 |
5,632 |
58.9% |
7,244 |
2,781 |
10,025 |
| 2015 |
4,947 |
58.0% |
6,395 |
2,549 |
8,944 |
| 2014 |
5,123 |
58.5% |
6,655 |
2,613 |
9,268 |
| 2013 |
5,142 |
60.4% |
6,494 |
2,118 |
8,612 |
| 2012 |
4,665 |
60.2% |
6,006 |
1,540 |
7,546 |
| 2011 |
4,557 |
60.2% |
5,766 |
1,828 |
7,594 |
|
Source: PHE, HIV/STI Portal, GUMCADv2 Report.
* During the COVID-19 pandemic sexual health services adapated delivery, offering more telephone consultations and online testing options. Fewer attendances during this period were 'face-to-face'. Whitegate Drive Clinic also acted as a hub for wider telephone and online testing requests across Lancashire, hence the low reported proportion of Blackpool residents.
|
Sexual Health Screens
There were 10,842 first attendances at all sexual health services by Blackpool residents in 2019. First attendances are new and re-booked appointments at the start of a new sexual health episode. 65% of these first attendances were female and those aged 20 to 34 made up over half (55.5%) of all attendances. 59% had a sexual health screen at first attendance (73% of males, 51% of females), that is where a combination of two or more of the following tests are taken: chlamydia, gonorrhoea, HIV and/or syphilis. Approximately 32% were diagnosed with a STI (figure 13). Sexual health screens taken at a follow-up attendance are not included in these figures.
Figure 13: Number of first attendances, screens and STI diagnoses, Blackpool residents, 2019
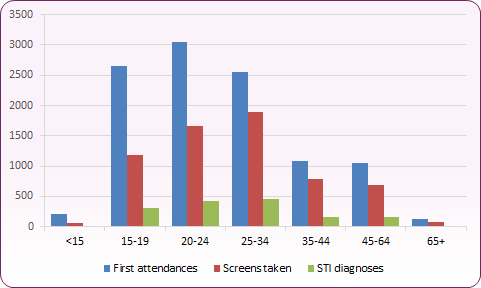 Source: PHE, HIV/STI Portal, GUMCADv2 Report
Source: PHE, HIV/STI Portal, GUMCADv2 Report
The number of first attendances and screens increased slightly between 2018 and 2019, with 6,389 screens in 2019 (compared to 5,927 in 2018). The proportion of first attendances receiving a screen remained stable at 59%. In 2020 first attendances dropped by 14% to 9,297, whilst screens fell 36% to 4,081, 44% of first attendances. The largest reduction in screens was among those aged under 19 (figure 14).
Figure 14: Trend in sexual health screens by age and gender, 2018-2020
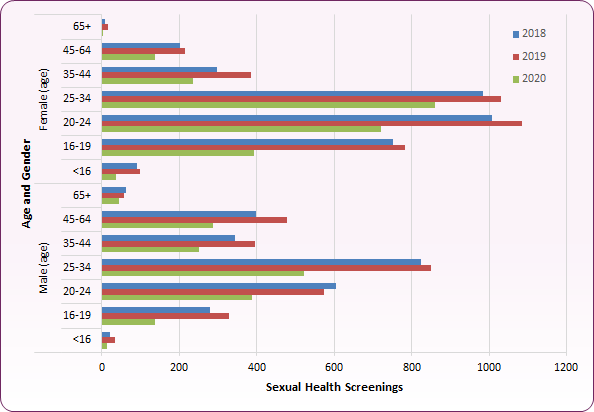 Source: PHE, HIV/STI Portal, GUMCADv2 Report
Source: PHE, HIV/STI Portal, GUMCADv2 Report
Tier 2 STI testing in Primary Care
The Tier 2 General Practitioner (GP) led Sexual Health Service was developed in 2007/08 to provide testing and treatment of sexually transmitted infections in the community - Level 2 STI services. The service was designed to complement the sexual health service available through GUM, with GUM taking on the role of training and governance and the treatment of the more complex sexual health conditions.
The service is currently provided by the following GP practices:
- Adelaide Street Surgery (Harris Medical Centre)
- Stonyhill Medical Centre
Figure 15: Location of each primary care Tier 2 service provider, including Connect and all age Sexual Health Services (Whitegate Health Centre)
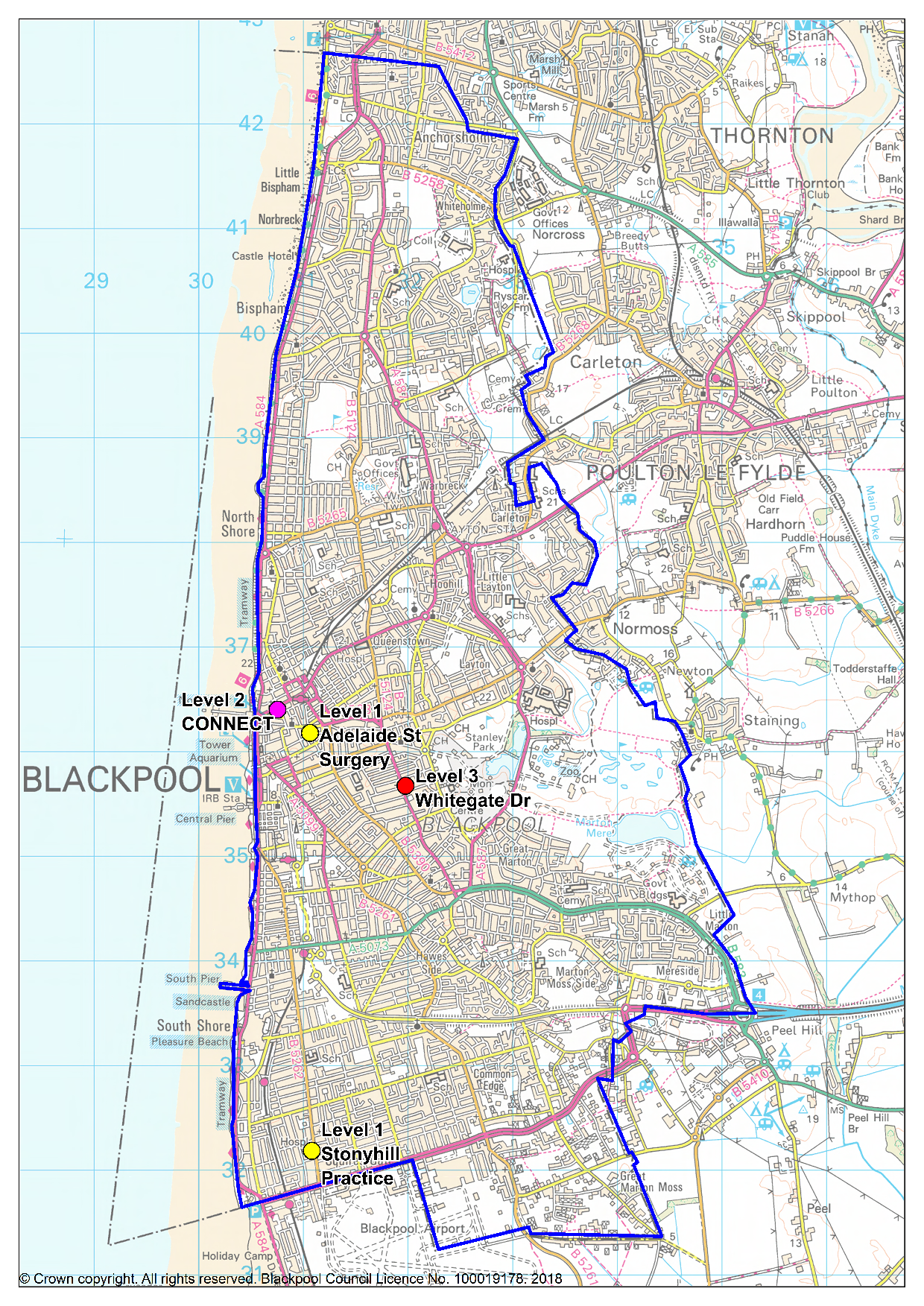 (For definitions of Level 1, Level 2 and Level 3 sexual health services see here)
(For definitions of Level 1, Level 2 and Level 3 sexual health services see here)
The service is open to any resident, whether registered at the practice or not. Patients testing positive at the Tier 2 service are treated, with partner notification undertaken. However, those testing positive for more complex conditions such as HIV, Syphilis and Gonorrhoea would be referred to the Tier 3/Level 3 service for treatment.
There are different models of delivery depending on the service provider - for example, GP-led or nurse-led, offering booked appointments and/or drop-ins. During a 'new appointment' (patient's first appointment), patients are offered a full STI screen.
Practitioners at all the delivery practices will manage symptomatic MSM and practitioners at all the practices will manage pregnant women with STIs. These are traditionally not managed in primary care but practitioners will consult with the Level 3 service and refer when necessary.
Around 85% of those presenting to the Tier 2 services for sexual health screening are asymptomatic, and positivity rates are low. The most common infection detected is chlamydia, together with some cases of gonorrhoea.
Tier 2 contraception in primary care
The Department of Health's Framework for Sexual Health Improvement in England includes the ambition to reduce unwanted pregnancies among all women of fertile age through:
-
- increased knowledge and awareness of all methods of contraception among all groups in the local population,
- increased access to all methods of contraception, including long-acting reversible contraception (LARC) methods and emergency hormonal contraception, for women of all ages and their partners.
The Public Health Outcomes Framework indicator of GP prescribed LARC (excluding injections) replaces an earlier indicator which included injections, because:
-
- injections rely on repeat visits/administration within the year and have a higher failure rate than the other LARC methods,
- injections are easily given in primary care and do not require the resources and training that other LARC methods require,
- injections are outside local authority contracts.
The 2019 rate per 1,000 women on long acting reversible contraception (LARC) prescribed in primary care was 22.5 for Blackpool, 21.7 for North West and 30 per 1,000 women in England (figure 16). However, this is prescribing data and may not include implants purchased through central supply of implants provided to the practices by the Integrated Sexual Health Service at Whitegate Drive.
Figure 16: Rate of GP prescribed long acting reversible contraception (LARC) excluding injections, Blackpool and England
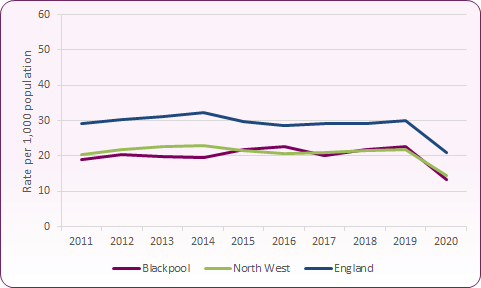 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
Emergency contraception can be used following unprotected intercourse, contraceptive failure, incorrect use of contraceptives, or in cases of sexual assault. It is intended for occasional or emergency use, not as a primary contraceptive method for routine use. Use of EHC is closely linked to a reduced rate of unplanned pregnancies for women of all ages and the availability of EHC is essential in reducing the teenage conception rate and also the number of unplanned pregnancies which result in termination.
In 2019/20, 940 Blackpool residents were provided with emergency contraceptives by Sexual and Reproductive Health Services, including 90 aged under 16 years. The rate of emergency contraceptive provision by SRH services in Blackpool was 21 per 1,000 women aged 13 to 54 - the highest in England (England rate was 5 per 1,000). For those aged 13 to 15 years, the rate was 32 per 1,000, the second highest in England (England rate 4 per 1,000). However, this comparative data does not include emergency contraception provided by primary care and pharmacies in some areas, and may also reflect the focus on a centralised, accessible sexual health service, particularly for young people through Connect Young People's Service. In 2019/20, primary care (GP surgeries) prescribed emergency hormonal contraception on 278 occasions. This is similar to the 2018/19 level (265).
EHC in pharmacy settings in some cases offers opportunities for easier access when young women may have been at risk from an unplanned pregnancy and sexually transmitted diseases (STIs). However, findings from a 2016 service review in Blackpool showed that few patients accessing community pharmacy were given the wrap around service they would receive from their GP or sexual health service, particularly in terms of STI screens and follow-on contraception. Not only are the majority of young people screened for STIs at the sexual health services, they also receive the contraception of their choice; with nearly 50% taking up long acting reversible contraception (LARC). Essentially, the demand for EHC from pharmacies from those under the age of 19 was found to be low in Blackpool, with most young people accessing EHC for free through Connect Young Peoples service. Following the review it was decided to discontinue the provision through pharmacies and provide all EHC through sexual health services and primary care.
Contraceptive care
Good contraception services have been shown to lower rates of teenage conceptions. Knowledge, access and choice for all men and women relating to all methods of contraception to aid in the reduction of unwanted pregnancies is supported by the government and the Faculty of Sexual and Reproductive Healthcare (FSRH).
In 2019/20, of 1.3 million attendances for contraceptive care at sexual health services by residents in England, 8,010 were by residents from Blackpool. The percentage of female residents in Blackpool accessing sexual health services for contraception is significantly higher than the England average (13% in 2019/20, compared to 5% across England). As is evident from figure 17, levels dropped considerably both locally and nationally during the 2020/21 Covid-19 period.
Compared to the national average, a greater proportion of attendees at contraception services are in the younger age groups. In 2019/20 30% of all women attending SRH services for contraception were under 20 years of age, compared to only 19% nationally.
Figure 17: Percentage of female resident population using SRH services for contraception, by age group: 2019/20 and 2020/21
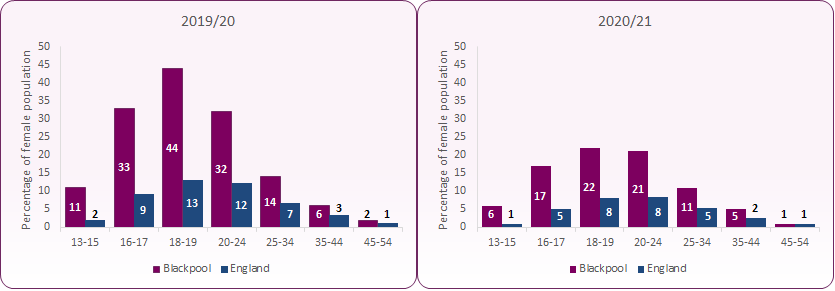 Source: NHS Digital, Statistics on Sexual and Reproductive Health Services (Contraception), 2019/20 and 2020/21
Source: NHS Digital, Statistics on Sexual and Reproductive Health Services (Contraception), 2019/20 and 2020/21
Long Acting Reversible Contraception (LARC)
In 2019, the rate of total LARCs prescribed to women aged 15 to 44 years in Blackpool was 74.2 per 1,000 in Blackpool, compared to 50.8 per 1,000 for England (figure 18). Blackpool's rate was the fourth highest in England. LARC fittings (and removals) declined considerably both nationally and locally during the Covid-19 'lockdown' in 2020 due to services reducing face-to-face consultations and adapting their contraceptive offer / protocols during this time.
Figure 18: Overall rate of long acting reversible contraception (LARC) excluding injections, Blackpool, North West and England
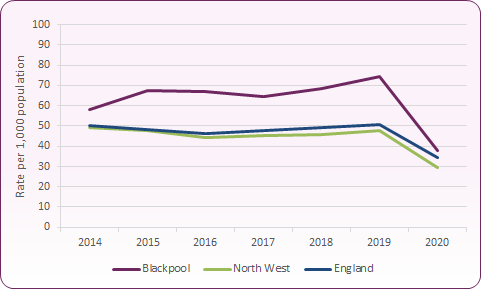 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
As figure 19 shows, Sexual Health Services account for a large proportion of LARC fittings in Blackpool, with 51.9 per 1,000 women prescribed LARC in 2019, compared to a rate of 20.8 per 1,000 nationally. Blackpool's rate for LARC prescribing within sexual health services is the highest in the country.
Figure 19: Rate of Sexual Health Service prescribed long acting reversible contraception (LARC) excluding injections, Blackpool, North West and England
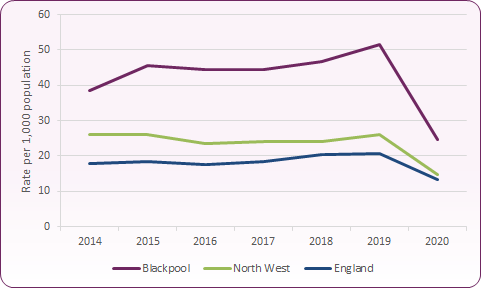 Source: PHE Sexual and Reproductive Health Profiles
Source: PHE Sexual and Reproductive Health Profiles
Figure 20 compares proportions of each contraceptive method prescribed to residents in Blackpool and England by sexual and reproductive health services. In 2019, of all contraceptive methods prescribed, the main methods of contraception for residents in Blackpool were 37.2% LARC (over 25s), 26.4% LARC (under 25s), 20.1% injectable contraception and 49.3% user dependent method (UDM). The proportion of women receiving injectable contraception Blackpool is significantly higher than the national average (9.4% in 2019).
Source: PHE Sexual and Reproductive Health Profiles
The number of LARCs reported is not necessarily an indication of compliance, since the contraception may be removed early for a range of reasons. Blackpool sexual health service data (figure 21) shows that in 2019/20 and 2020/21, a significant number of women in Blackpool have had the hormonal contraceptive implant (which can last up to 3 years) removed compared to other LARC methods. This is also reflected in previous years' data: in 2014, Blackpool SRH services showed a higher proportion of women were having the implant removed, 5.5 compared to 2.3 and 2.7 in the NW and England respectively4. An audit of the number of early removals will be required to better understand compliance with the method.
Attitudes to Sexual Health - National Survey of Sexual Attitudes and Lifestyles (Natsal)
Due to the cost and complexity of such studies, limited work has been undertaken locally to determine the trends in attitudes to sexual health. Hence, information is drawn from national studies, such as the National Survey of Sexual Attitudes and Lifestyles (Natsal) 2013. This was the third survey carried out in Britain and the researchers interviewed 15,162 men and women aged 26-74 between September 2010 and August 2012.
Over the 1990's, there was an increase in the number of opposite sex partners people reported and more people reporting same sex experience. Over the last decade there have been further increases for women, so the gender gap is narrowing. The percentage of people reporting sexual intercourse with someone of the opposite sex before the age of 16 has not increased substantially since the mid 1990's (figure 22), with approximately 1 in 3 young people reportedly having sex before the age of 16.
Figure 22: Percentage of the population who have ever had same sex experience and sexual intercourse with someone of the opposite sex before age 16
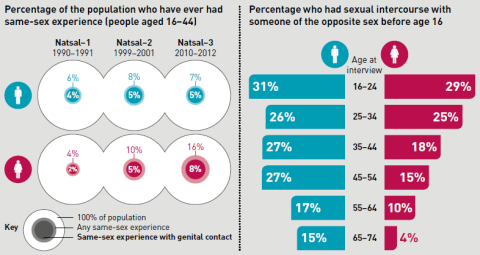 Source: NATSAL Survey 2013
Source: NATSAL Survey 2013
Data from the survey provides the first population prevalence estimates of non-volitional sex in Britain. Non volitional sex is a term which includes coercion, sexual assault and rape by friends, partners or strangers, i.e. sex against your will since the age of 13. In most cases the person responsible was someone known to the individual (figure 23). This was the first of the NATSAL surveys to include questions on sexual violence (outside the context of crime) and was strongly associated with a range of adverse health outcomes in both men and women.
Figure 23: Person responsible at most recent occurrence of sexual violence
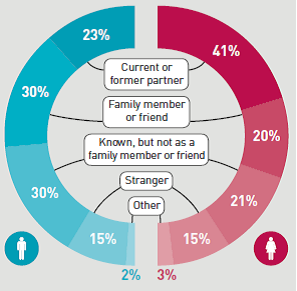 Source: NATSAL Survey 2013
Source: NATSAL Survey 2013
Over the past decade, national sexual health strategies in Britain have aimed to increase access to sexual health services and STI/HIV testing. Compared with previous surveys, more people reported having an HIV test or going to a sexual health clinic in the past 5 years. It is encouraging to see that these increases were even larger in those at highest risk, such as people who reported multiple partners.
The researchers found that unplanned pregnancy was less common than has been found in studies done in some other high income countries such as the USA. This may in part reflect the fact that contraception is provided free of charge in Britain under the NHS.
Sexual lifestyles in Britain have changed substantially in the past 60 years, with changes in behaviour ostensibly more evident in women than men. The continuation of sexual activity into later life emphasises that consideration of sexual health and wellbeing is needed throughout the life course.
Condom use and the use of contraception had increased over the period of the three studies. The main source of sexual health education is now schools. In the 1990 survey most advice was sourced from friends.
While most people have had vaginal sex in the past year, other practices are less common, especially anal sex. Anal sex was most frequently reported by young people. This is important in relation to communicating the risk of HIV in both the younger heterosexual population and men who have sex with men.
According to the survey, overall, around one in a hundred people aged 16-44 had Chlamydia, although this varied by age, peaking at almost one in twenty women aged 18-19 and one in thirty men aged 20-24. Although people who reported more partners in the past year were more likely to have Chlamydia, Chlamydia was found in people who reported only one partner in the past year.
The percentage of men reporting the use of sex workers in the past five years was 4% with 0.1% of women (4 in 100 men and 1 in 1,000 women).
Renaissance at Drugline Lancashire: Sexual Health Services in Blackpool
Renaissance at Drugline Lancashire provides a range of harm reduction services including non-clinical, co-ordinated support for individuals who are living with or who are affected by HIV, Hepatitis C or affected by sexual violence. This includes the lesbian, gay, bisexual and transgender (LGBT) community and populations at high risk of poor sexual health, for example, sex workers and men who have sex with men (MSM). As part of the Horizon Project, Renaissance supports the needs of the LGB&T community, particularly around sexual health issues and have targeted work with peer support groups for Trans community members as well as LG&B social and support groups. The LGB&T Development Leads also coordinate a team of sexual health outreach workers that offer community interventions in LGB&T focused venues as well as saunas and public sex environments.
Renaissance also provides sexual health information, advice and support to those involved in sex work across Blackpool, particularly through outreach into parlours across the resort.
Under GUM governance, Renaissance provides HIV insti-testing as part of the Public Health England MSM testing programme in venues throughout the town. The 'Insti' 60 second HIV tests have also resulted in some reactive results, with onward referral for confirmatory serological test.
Sexual exploitation, violence and abuse
Sexual and domestic violence and sexual exploitation and abuse can be issues for men, women and children. The Crime Survey for England and Wales (CSEW) reported that 26.6% of the 58,845 rapes recorded by the police in England and Wales in 2019/20 were committed against children under 16 years of age, and 73,260 sexual offences were recorded where the victim was a child. In 2013 Stonewall found that 49% of gay and bisexual men have experienced at least one incident of domestic abuse from a family member or partner since the age of 16, and 25% of lesbians and bisexual women have experienced domestic violence in a relationship6,7. Service providers should be alert to these issues and be able to provide support and make onward referral for victims including to the police, social services and specialist health and third sector services.
Although routine enquiry about domestic violence in pregnancy has been undertaken for a number of years in antenatal settings, there has been less focus on screening in women having an abortion. Studies show an association between domestic violence and termination (and repeat termination) of pregnancy8. Evidence shows that such violence can severely affect the mental and sexual and reproductive health of victims9.
Across Blackpool:
-
- Abuse and neglect represent the biggest need areas for safeguarding children in Blackpool and proportions of children in need are higher than seen elsewhere;
-
- Although low in volume, rape has the greatest impact in terms of harm in Blackpool.
- Mental illness can impact on sexual behaviour, impairing judgement, especially for individuals dependent on alcohol and other substances;
- Self-report of STIs, termination of pregnancy and sexual assault are high in sex workers;
- Poor access to sexual health services for sections of our society who need it the most.
In 2021 there were 902 recorded sexual offences in Blackpool, an increase of 37% compared to 2020. Rape offences increased by 45% and sexual offences against children under the age of 16 increased by 25%10. It appears that the 2020 and 2021 COVID-19 lockdown periods impacted on these figures, with fewer offences in 2020 offset by an increase in 2021. Blackpool's recorded crime rate for sexual offences in 2020/21 was 4.8 per 1,000, one of the highest rates in the country11.
It is widely acknowledged that reliable information on the volume of sexual offences is difficult to obtain because a high proportion of offences are not reported to the police. However, we need to ensure that sexual violence pathways for reporting, referral and support are available to all agencies, and there is equity of provision. Rape is not a gender specific issue but evidence does suggest it disproportionately affects females. The Tackling Violence against Women and Girls Strategy12 aims to increase awareness in children and young people of respect and consent in relationships and that abusive behaviour is wrong - including abuse taking place on line.
Overall, there is a correlation between sexual health and other key determinants of health and wellbeing, such as alcohol and drug misuse, mental health and violence (particularly violence against women and girls), contributing to a reduction in health inequalities.
New and emerging trends and developments
'Chemsex'
An emerging trend of sexualised drug use has been identified. Chemsex is a commonly used term to describe sex under the influence of drugs taken immediately before and/or during sexual contact. It is a rapidly emerging pattern of drug use, not just amongst men who have sex with men as often assumed, but heterosexual people as well13. The main drugs chemsex refers to are GHB/GBL14, mephedrone, crystal meth, cocaine and ketamine. Use of these drugs by gay men in London appears to have risen sharply from relatively low levels but, as yet, there is little data from services to suggest that chemsex is a significant concern in Blackpool.
The risk of chemsex drugs can be:
-
- having sex with more people than planned
- Within the gay community there is an increased risk of unprotected anal and rough sex
- Chemsex can prolong sex sessions giving an increased opportunity for infections to be passed on, so people may be at risk of getting an STI
- Sharing of needles to inject with can spread diseases and injecting may increase risk of overdosing
- Shigella is a bacterium which has been linked to gay men who use chemsex drugs.
Pre-exposure prophylaxis (PrEP)
Pre-exposure prophylaxis (PrEP) is a course of HIV drugs taken before sex to reduce the risk of getting HIV. Following a trial involving 10,000 people in England (including some in Blackpool), PrEP is now available free on the NHS in England from sexual health clinics. The UK's PROUD study reported an 86% reduction in HIV infections in gay men taking PrEP15.
HPV Vaccine for MSM and Transgender People
HPV is one of the most common sexually transmitted infections in the UK, and can be caught through any kind of sexual contact with another person who already has it. Since 2018 men who have sex with men up to and including 45 years of age have been eligible for free HPV vaccination on the NHS when they visit sexual health clinics. Trans women (people who were assigned male at birth) are eligible in the same way if their HPV transmission risk is similar to that of eligible MSM. Trans men (people who were assigned female at birth) are eligible if they have sex with other men and are aged 45 or under.
Blackpool has the highest rate of LAC within England and has far higher rates than similar local authorities. Data at March 2020 showed 652 children were looked after in Blackpool. The rate of LAC was 223 per 10,000 children under 18 compared to the national average of 67 per 10,00016.
The available evidence shows that children in care often have a higher rate of poor sexual health and may be more prone to involvement in risky sexual activity, exploitive and abusive relationships and early parenthood. Many looked after young people in Blackpool may also have come to Blackpool from other areas in the region and beyond and as such are likely to have little or no knowledge of local services.
Although it is currently impossible to accurately calculate the prevalence of Child Sexual Exploitation (CSE) at a national or local level, CSE remains an issue in Blackpool and across Lancashire. For further information about CSE in Blackpool, visit the Blackpool JSNA CSE webpage.
Sex workers
Blackpool has a number of sex workers operating on the street, as well as in venues such as massage parlours and saunas. Sex workers as a group can be characterised by multiple vulnerabilities, for example, having been a looked after child or young person17 or having drug or alcohol problems18. Self-report of sexually transmitted infections (STIs), termination of pregnancy and sexual assault are also high in this group19. It is vital that the sexual health needs of this vulnerable group are prioritised in any sexual health strategy.
Operation Azure is a multi-agency partnership formed to tackle issues around sex work in Blackpool. This includes preventing the sexual exploitation of women and children and dealing with premises which are nuisances to the public.
The Sex Workers Outreach and Support Service (SWOSS) project is funded by Blackpool Council and provided by Renaissance at Drugline, Lancashire. The service supports all those over the age of 18 involved in the sex industry in Blackpool. This includes the provisions of free condoms, help with accessing sexual health and other health services, support with substance misuse issues and promotion of personal safety, sexual health and emotional health and wellbeing. Additionally, the service promotes the Ugly Mugs scheme, allowing sex workers to circulate descriptions of dangerous customers nationwide.
Lesbian, Gay, Bisexual and Transgender
Blackpool has a large lesbian, gay, bisexual and transgender (LGBT) community. Accurate estimates of the numbers in the population are difficult to arrive at, although sexual orientation is now recorded in the national census. Local estimates have provided a figure of 7-8% of the population in Blackpool being lesbian, gay, bisexual or transgender (national estimates based on the Integrated Household Survey 2012 are 1.5%) which would give a figure of around 10,500 LGBT people in Blackpool. Blackpool has a large number of LGBT businesses such as entertainment venues, hotels and guesthouses, all of which attract visitors from outside of the area. It should also be noted that Blackpool's LGBT population is as likely to be affected by issues of transience and migration in and out of the area as is the rest of Blackpool's population.
Lesbian, gay, bisexual and transgender people experience a number of health inequalities which are often unrecognised in health and social care settings. Research suggests that discrimination has a negative impact on the health of LGBT people. Many people are reluctant to disclose their sexual orientation to their healthcare worker because they fear discrimination or poor treatment. Healthcare and other professionals commonly assume that LGBT people's health needs are the same as those of heterosexual people. The sexual health needs for LGBT people are not homogeneous. Lesbians, gay men, bisexual men and women, transgender men and women, young LGBT people and older LGBT people will all have differing needs. Research commissioned by Stonewall indicates that a high proportion of lesbian and bisexual women6 and gay and bisexual men7 have never been tested for STIs.
Evidence also suggests that gay and bisexual men who use particular illegal drugs (as well as alcohol) are more likely to engage in risky sex. Stonewall's 2013 research found that 51% of gay men had taken illegal drugs in the previous year, compared with 12% of men in the wider population.
Services should ensure that they are accessible and welcoming to LGBT people. Services should ensure all staff undertake training to understand the varying needs and potential barriers to access for LGBT people and are able to actively challenge homophobia. Services should outreach to LGBT groups and venues to increase awareness of their services. All sexual health services should maintain close links with local LGBT community groups, youth groups and voluntary sector organisations. There is a particular need for sexual health materials such as posters and leaflets specifically for young LGBT people in Blackpool. Much of the available materials are not age appropriate or are specific to other areas of the country.
All sexual health services should give careful consideration to routinely monitoring the sexual orientation of their clients. This will enable services to ensure they are accessible to this group.
Prison Population
Blackpool does not have a prison, though Kirkham prison is located close by. This presents a number of challenges particularly related to sexual health for prisoners who are on day release and choose to spend their time in Blackpool. This has placed a significant burden on prison health care in treating associated infections.
Vulnerable Adults (including Learning Disabilities)
Coping with puberty, sexual identity and sexual feelings can be more difficult for people with learning disabilities who might be struggling to understand their emotions and their body. The sexual needs of people with learning disabilities have historically been ignored and, often, sexuality only becomes an issue to be discussed when there is a problem.
Sexual health services in Blackpool aim to improve access to services for people with a learning disability/mental health issue by working with mental health and learning disability teams to develop domiciliary care pathways for vulnerable groups not accessing services.
Service provision is also targeted at groups with particular needs who may be vulnerable and at risk from poor sexual health, including young people, gay and bisexual men, some black and minority ethnic groups as well as people with learning disabilities.
Blackpool's main clinical sexual health service is delivered from Whitegate Health Centre. This includes the provision of an open access Tier 1,2 and 3 service which is open to anyone of any age, irrespective of where they live. Elements of a Tier 1 service include the provision of emergency oral contraception, sexual history taking and Chlamydia testing, with Tier 3 involving management of complex contraceptive problems and specialised infections management.
Connect Young People's Service provide a Tier 2 open access clinical service for anyone aged under 25, which includes STI screening, contraception and management of uncomplicated infections. Two GP Practices have also been commissioned to provide Tier 2 sexual health services for Blackpool residents.
In recent years, investment has been made through Public Health to improve access to Blackpool sexual health services, including easier access for high-risk groups. This investment includes the development of the following:
- Staff in Primary care have been trained to fit and remove contraceptive implants, intrauterine systems/devices and local enhanced service agreements are in place with a number of GP practices in Blackpool for both their registered and non-registered patients. These LARCs (long acting reversible contraceptive) are more reliable than user-dependent methods like oral contraceptives and less likely to lead to unintended conceptions
- A young people's sexual health/substance misuse harm reduction service has been commissioned, which includes training on risky behaviour for frontline workers working with young people and provision of a bus to enable young people to access harm reduction messages and Chlamydia testing
- Chlamydia testing is offered by harm reduction and other services accessed by people aged under 25
- A condom distribution scheme is in place, with a particular focus on men who have sex with men (MSM) by providing free condoms and lubricant through outreach in public sex environments and pubs and clubs
- Outreach visits to children's homes to enable Looked After Children to access contraception and sexual health services
- Targeted work with sex workers to facilitate access to sexual health services
- Sexual health services are delivered through non-clinical settings such as saunas and within Horizon drug and alcohol treatment services
- A PSHE Support Officer works with schools to develop RSHE provision and give RSHE / PSHE school leads a network of best practice, access to training and a suite of quality assured schemes of work, lesson plans and resources.
- Access to HIV testing is being increased through Accident & Emergency (A&E), GP practices, point of care testing in community venues and home self-sampling
[] WHO (2006) Defining sexual health: Report of a technical consultation on sexual health, 28-31 January 2002, Geneva, http://www.who.int/reproductivehealth/publications/sexual_health/defining_sexual_health.pdf
[] PHE, Health Protection Report, Vol 10 Number 22. Sexually transmitted infections and chlamydia screening in England, 2020
[] PHE, Addressing the increase in syphilis in England: PHE Action Plan, June 2019.
[] PHE, Blackpool Summary Profile of Local Authority Sexual Health (SPLASH): 2021
[] PHE, Trends in HIV testing, new diagnoses and people receiving HIV-related care in the United Kingdom: data to the end December 2019.
Stonewall (2013) Lesbian and Bisexual Women's Health Survey
Stonewall (2013) Gay and Bisexual Men's Health Survey
Aston G and Bewley S, Abortion and domestic violence, The Obstetrician and Gynaecologist 2009; 11:163-8
Dept of Health, A Framework for Sexual Health Improvement in England (2013)
Blackpool Community Safety Partnership. Blackpool Community Safety Plan 2022-2025.
Office for National Statistics, Recorded crime data by Community Safety Partnership: Year ending March 2021.
HM Govt, Tackling Violence against Women and Girls Strategy, Updated 2021.
BMJ Editorial, What is chemsex and why does it matter? BMJ 2015; 351:h5790
GHB (gammahydroxybutrate) and GBL (gammabutyrolactone), are closely related, dangerous drugs with similar sedative and anaesthetic effects. GBL is converted to GHB shortly after entering the body. Both produce a feeling of euphoria and can reduce inhibitions and cause sleepiness.
Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial McCormack, Sheena et al.The Lancet , Volume 387 , Issue 10013 , 53 - 60
Office of National Statistics (ONS), Children looked after in England including adoptions, reporting year 2019/20.
Jeal N. and Salisbury C (2004) Health Needs Assessment of Street-based Prostitutes. Journal of Public Health (Oxford) 2004 Jun;26(2):147-51
Pinkham S. Stoicescu C. and Myers B. (2012) Developing Effective Health Interventions for Women who Inject Drugs: Key areas and recommendations for programme development and policy. Advances in Preventative Medicine, 2012 Vol 2012 Hindawi Publishing Corp.
Edelman L. Patel H. Glasper A. and Bogen-Johnston L. (2014) Original Research Sexual Health Risks and Health-seeking Behaviour among Substance-misusing Women. Journal of Advanced Nursing. John Wiley and Sons Ltd