Childhood Immunisations (5 years and over)
Last Modified 28/03/2023 11:42:43
Share this page
Introduction
After clean water, vaccination is the most effective public health intervention in the world for saving lives and promoting good health. Immunisation is the most essential way of protecting people and communities from serious infectious diseases. As well as the individual being protected themselves, vaccinated people are also less likely to be a source of infection to others.
Many vaccine-preventable childhood diseases are now so rare that it is easy to underestimate the importance of children's vaccinations. However, whooping cough and diphtheria are still a threat. The diseases are rare now, but if children are not vaccinated, they can return with a vengeance.
Currently the European Region of the World Health Organization (WHO) recommends that on a national basis at least 95% of children are immunised against diseases preventable by immunisation and targeted for elimination or control (specifically, diphtheria, tetanus, pertussis, polio, Hib, measles, mumps and rubella)1. The routine childhood immunisation programme for the UK includes these immunisations recommended by WHO as well as a number of others as defined by the UK Health Security Agency (UKHSA). The complete routine immunisation schedule is published annually by the UK Health Security Agency and is available at the link below:
Childhood immunisations (0-4 years) and adult vaccinations provides data on younger children and adults. Further information on infectious diseases and other noncommunicable health threats is available in the Health Protection section.
Facts, figures and trends
In addition to OHID Public Health Profiles, vaccination coverage data can be accessed via two experimental interactive dashboards:
Note: The COVID-19 period has impacted vaccination and immunisations programmes in a number of ways. During the COVID-19 period, coverage for some vaccinations dropped across the country, for example in relation to measles, mumps and rubella (MMR) vaccination. Although some catch-up is underway the UK Heath Security Agency has warned that susceptibility will have increased in recent years, with the potential of larger outbreaks.
2020/21 data published by NHS England shows that in Blackpool:
-
- The number of children who had received the Haemophilus influenza type b and meningitis C (Hib/MenC) booster by age 5 years was 1,787 (94.5%)
- The number of children who received the combined Diptheira, Tetanus, Polio, Pertussis and Hib primary vaccine by age 5 year was 1,825 (96.5%)
- The number of children who had received the measles, mumps and rubella (MMR) vaccine, 1 dose, by age 5 years was 1,813 (95.9%)
- The number of children who had received the measles, mumps and rubella (MMR) vaccine, 2 doses at age 5 years was 1,687 (89.2%)
Figure 1: Percent of children immunised by their 5th birthday: 2020/21
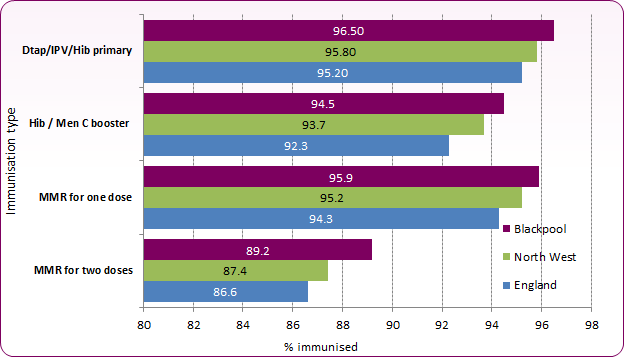 Source: OHID, Public Health Profiles
Source: OHID, Public Health Profiles
Figure 2: Trend in proportion of children immunised by their 5th birthday
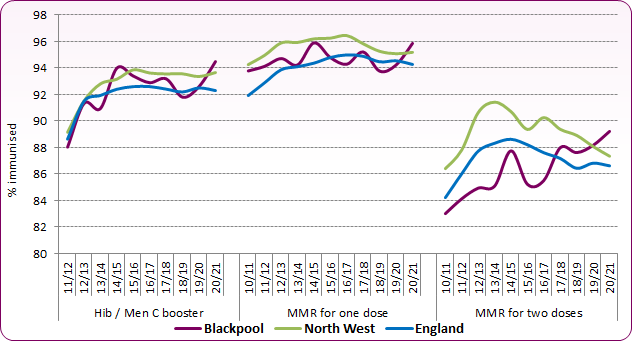 Source: OHID, Public Health Profiles
Source: OHID, Public Health Profiles
Across Blackpool, immunisation uptake by the age of 5 years is slightly higher than the national average for the Hib/Men C booster and is above the 90% goal for this and for one dose of the MMR vaccine. However, two doses of MMR vaccine are required to provide satisfactory protection against measles, mumps and rubella4, and although coverage in Blackpool is now above the national average (Figure 1) it remains below the goal of 90%. In 2020/21, 89.2% of Blackpool's children had two doses of the MMR vaccine by the time they began school, an increase on recent years. Approximately 5%-10% of children are not fully immune after only one dose of the vaccine, therefore the second dose provides a further opportunity to protect children, with less than 1% of children remaining susceptible after receiving the two recommended doses2.
Figure 3 shows the longer term trend in the proportion of children who have received two doses of the MMR vaccine by their 5th birthday. In Blackpool coverage went from higher than the national average in 2005/06 to lower than the national average until 2019-20. In recent years, Blackpool's coverage level has risen, whilst national coverage has fallen. The increase in coverage in 2008/09 and 2009/10 was due to a 'catch-up' campaign at the time.
Figure 3: Trend in the proportion of children who have 2 doses of MMR vaccine by their 5th birthday
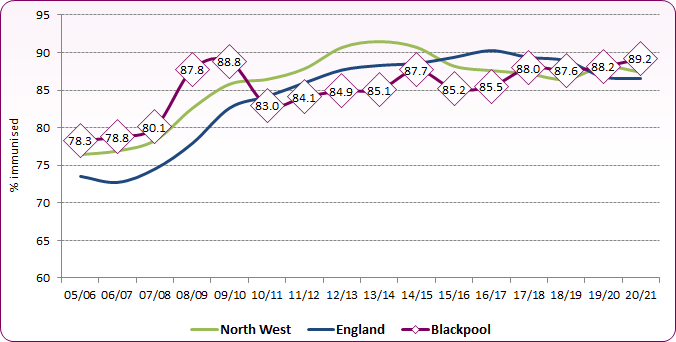 Source: NHS Digital, Childhood Vaccination Coverage Statistics
Source: NHS Digital, Childhood Vaccination Coverage Statistics
Figure 4 compares Blackpool with other local authorities in England. Blackpool ranks 77th out of 147 authorities with reported statistics and is in the third (middle) quintile for coverage.
Figure 4: Proportion of children who have 2 doses of MMR vaccine by their 5th birthday, comparison showing Blackpool with upper tier local authorities in England, 2020/21
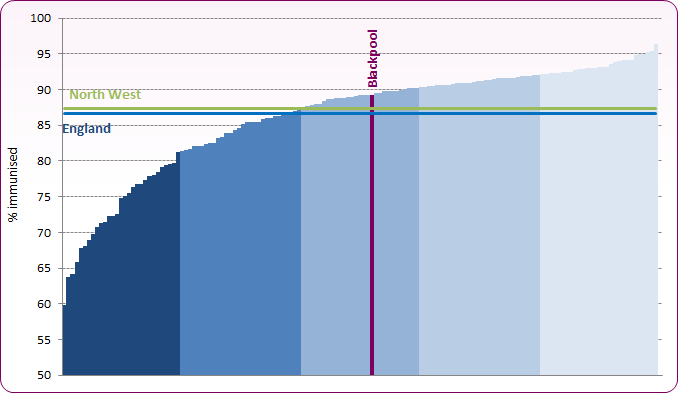 Source: NHS Digital, Childhood Vaccination Coverage Statistics
Source: NHS Digital, Childhood Vaccination Coverage Statistics
National data reported that there were 4,287 lab-confirmed cases of mumps in England in 2021, compared to 1,066 cases in 2018. Whilst this national rise has largely been caused by outbreaks amongst unvaccinated young adults attending college or university, it highlights the importance of ensuring that children are up-to-date with the MMR vaccination. Following reductions in MMR vaccination coverage during the COVID-19 period, in February 2002 the UK Health Security Agency (UKHSA) and the NHS launched a campaign calling on parents and guardians to ensure that children are up to date with the MMR vaccine and all other routine childhood vaccinations.
The HPV vaccine protects against two types of HPV virus (HPV-16 and HPV-18) which together are responsible for about 70% of cervical cancers. In addition, the vaccine can also protect against HPV-6 and HPV-11, the two strains of HPV that cause most cases of genital warts.
Since 2008, all 12 to 13 year old females (school year 8) in the UK have been offered the human papilloma virus (HPV) vaccination through the national HPV immunisation programme. For the 2019/20 school year HPV vaccination was also extended to males aged 12 to 13. The national human papillomavirus (HPV) immunisation programme was initially a three dose vaccination programme. Following expert advice it was run as a two-dose schedule from September 2014.
Please note: Due to the COVID-19 pandemic, all educational settings were closed from the 23 March 2020 and the delivery of the 2019/20 school immunisation programmes was paused, in line with UK Government COVID-19 guidance. As shown in the figures presented below, this has had a significant impact on the uptake of the HPV vaccination programme.
In Blackpool in 2018/19:
- 89.5% (522) of girls aged 12 to 13 years received their first dose vaccination for HPV
- 87.6% (602) of girls aged 13 to 14 years received their second dose vaccination for HPV
In the Covid-affected 2019/20 school year:
- 81.8% (530) of girls aged 12 to 13 years received their first dose vaccination for HPV
- 83.8% (486) of girls aged 13 to 14 years received their second dose vaccination for HPV
- 77.6% (562) of males aged 12 to 13 years received their first dose vaccination for HPV
In Covid-affected 2020/21:
- 72.4% (501) of girls aged 12 to 13 years received their first dose vaccination for HPV
- 80.1% (520) of girls aged 13 to 14 years received their second dose vaccination for HPV
- 64.7% (467) of males aged 12 to 13 years received their first dose vaccination for HPV
Coverage is higher than national and regional averages (Figure 5). Until the 2018/19 Covid impact, vaccination coverage had increased since 2016/17 following a decline from the peaks in 2014/15 (one dose) and 2015/16 (two doses) (Figure 6).
Figure 5: Proportion of children aged 12-13 and 13-14 receiving HPV vaccine 2020/21
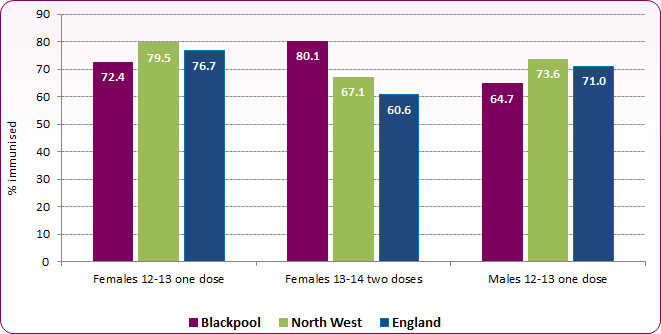 Source: OHID, Public Health Profiles / NHS Digital Childhood Vaccination Statistics
Source: OHID, Public Health Profiles / NHS Digital Childhood Vaccination Statistics
Figure 6 : Trend in proportion of females aged 12-13 (one dose) and 13-14 (two doses) receiving HPV vaccine
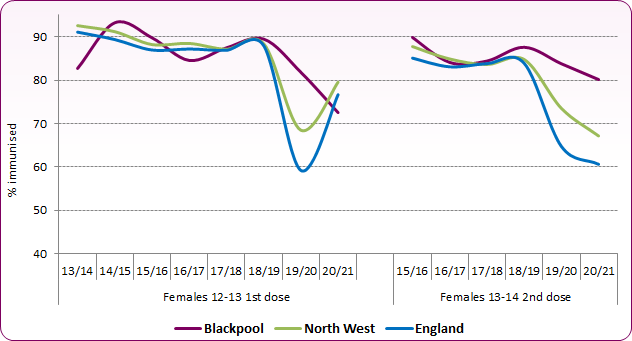 Source: OHID, Public Health Profiles / NHS Digital Childhood Vaccination Statistics
Source: OHID, Public Health Profiles / NHS Digital Childhood Vaccination Statistics
It is important that coverage is maintained as reductions in the prevalence of HPV 16-18 infections are consistent with very high vaccine effectiveness among those vaccinated and suggest that herd-protection is also lowering prevalence among those who are not vaccinated. Early findings from PHE support the expectation that vaccination will impact on cervical cancer and other HPV-related diseases in due course3 and it is anticipated that, with the new two-dose schedule, higher coverage of the completed course should be achievable, thus increasing the potential impact of the programme.
Influenza
In 2012 the Joint Committee on Vaccination and Immunisation (JCVI) recommended that the flu vaccination programme should be extended to all children aged two to 16 years old. The phased introduction of the programme to children began in 2013/14, with rollout to primary schools beginning in 2015/16. All primary school-aged children were offered the vaccine from the 2019/20 season onwards. In 2021/22 the national ambition was to achieve at least 70% vaccine uptake in 4 to 11 year olds.
COVID-19 affected school-based immunisation programmes across the country, however Blackpool saw a larger reduction in the proportion of vaccinated children in 2021 than that experienced across England or the North West Region. In 2021, 5,102 children in Blackpool received a flu vaccination (42.6%) compared to 7,234 (60.6%) the previous year (Figure 7).
Figure 7: Influenza Vaccination Coverage Trend (Primary School ages 4 to 11)
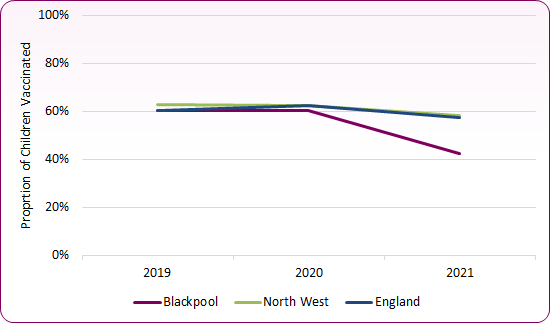
Source: OHID, Public Health Profiles
Variation within Blackpool
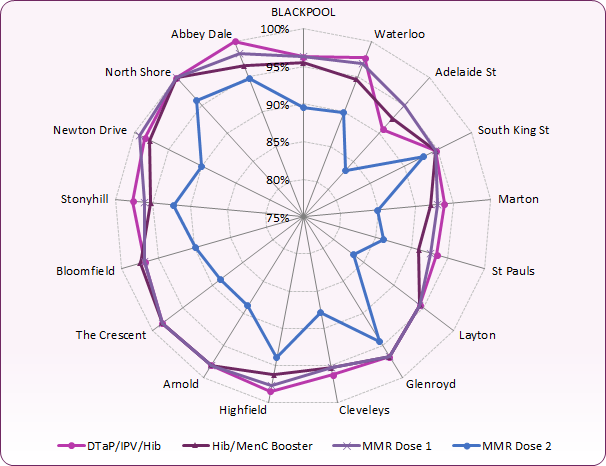
At a local level, there is variation in the proportion of children immunised in each of Blackpool's GP practices, with several practices having rates significantly lower than the Blackpool average. Figure 8 shows immunisations by the age of 5 years and the proportion of children immunised by each practice in 2020/21. Figure 9 shows proportions immunised by the age of 5 years for selected diseases.
Figure 8: Child Immunisations by the age of 5 years by GP Practice in Blackpool, 2020/21
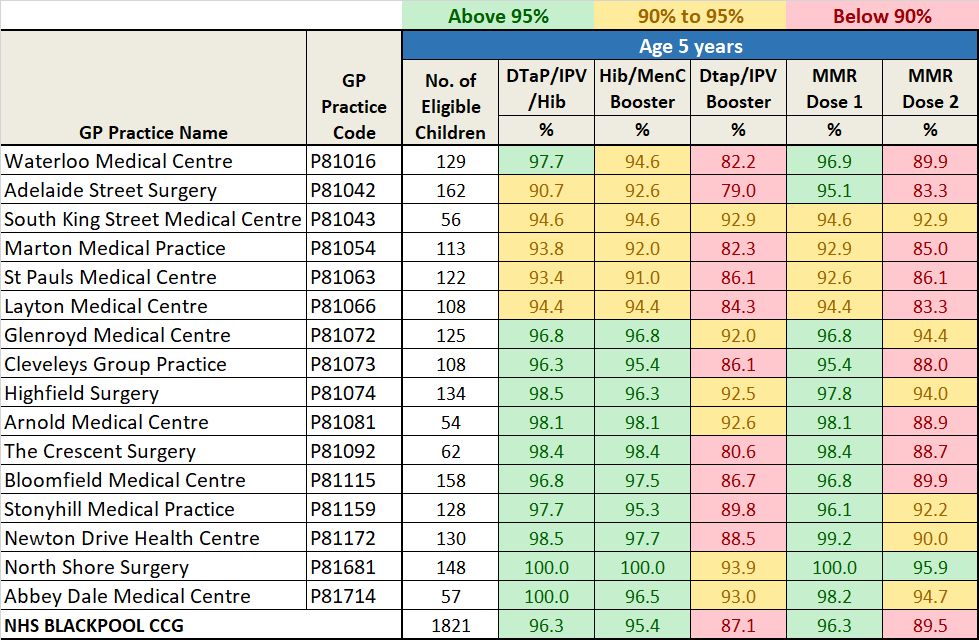 Source: NHS England, Child Immunisation by GP Practice
Source: NHS England, Child Immunisation by GP Practice
Figure 9: Proportion immunised for Dtap/IPV, Hib/Men C booster and MMR Doses 1 and 2 by the age of 5 years in Blackpool by GP practice, 2020/21
 Source: NHS England, Child Immunisation by GP Practice
Source: NHS England, Child Immunisation by GP Practice
In recent years there has been a renewed focus on improving outcomes for looked-after children and young people and one of the first standards to be published was to promote the health and wellbeing of looked-after children and young people4. Looked after children in Blackpool are significantly more likely to be up to date with their immunisations: in 2021, 94% of children in care for at least 12 months had all their immunisations compared to 86% nationally.
Risks
There are many reasons why people choose not to immunise themselves or their children. Studies have looked into how parents make decisions on whether to vaccinate their children or not and found that this is related to gaps in their knowledge of vaccine-preventable diseases, concerns over vaccine safety, and their attitudes towards immunisations, health professionals and health organisations.
Blackpool recognises that there is a need to target both overall improvement of immunisation coverage and specifically to improve the low levels of coverage amongst certain groups and in certain places.
Evidence has shown that the following groups of children and young people are at risk of not being fully immunised5:
• those who have missed previous vaccinations (as a result of parental choice or otherwise)
• looked after children
• those with physical or learning disabilities
• children of teenage or lone parents
• those not registered with a GP
• younger children from large families
• children who are hospitalised or have a chronic illness
• those from some minority ethnic groups
• those from non-English speaking families
• vulnerable children, such as those whose families are Gypsy Travellers, asylum seekers or are homeless.
National and local strategies
Department of Health (2013) immunisation information for health professionals and immunisation practitioners
The 'Green Book' has the latest information on vaccines and vaccination procedures, for vaccine-preventable infectious diseases in the UK.
The Complete Immunisation Schedule in the UK includes the ages of when the vaccines should be given.
In September 2009 the National Institute for Health and Clinical Excellence (NICE) published public health guidance 'Reducing the difference in the uptake of immunisations' which focuses on increasing immunisation uptake among children and young people aged under 19 years in groups and settings where immunisation coverage is low.
Department of Health (2009) Healthy Child Programme sets out the universal programme to be commissioned and provided for all families.
Public Health England's vaccination and immunisation snapshot provides a summary of demand, risk factors, provision and outcomes for services in a particular area.
[] Source: WHO, Health 21 The health for all policy framework for the WHO European Region, 1999
DH, 2014, NHS public health functions agreement 2015-16, Service specification No.10, Measles, mumps and rubella (MMR) immunisation programme
] PHE, Human Papillomavirus (HPV) Vaccine Coverage in England, 2008/09 to 2013/14. A review of the full six years of the three-dose schedule, March 2015
[] NICE Quality Standard 31(6) Looked-after children and young people: Tailored resource for corporate parents and providers on health and wellbeing of looked-after children and young people
[] NICE. Reducing differences in the uptake of immunisations (including targeted vaccines) among children and young people aged under 19 years. London: National Institute for Health and Clinical Excellence; 2009