Childhood Immunisations (0-4 years)
Last Modified 16/11/2023 12:28:08
Share this page
Introduction
After clean water, vaccination is the most effective public health intervention in the world for saving lives and promoting good health. Immunisation is the most essential way of protecting people and communities from serious infectious diseases: as well as the individual being protected themselves, vaccinated people are also less likely to be a source of infection to others.
Many vaccine-preventable childhood diseases are now so rare that it is easy to underestimate the importance of children's vaccinations. However, whooping cough and diphtheria are still a threat. The diseases are rare now, but if children are not vaccinated, they can return with a vengeance.
Currently the European Region of the World Health Organization (WHO) recommends that on a national basis at least 95% of children are immunised against diseases preventable by immunisation and targeted for elimination or control (specifically, diphtheria, tetanus, pertussis, polio, Hib, measles, mumps and rubella)1. The routine childhood immunisation programme for the UK includes these immunisations recommended by WHO as well as a number of others as defined by the UK Health Security Agency (UKHSA) and the complete routine immunisation schedule for health professionals and immunisation practitioners is published annually by UKHSA.
There are also selective childhood immunisation programmes that target children at particular risk of certain diseases, such as tuberculosis (TB).
Childhood immunisations (5 years and over) and adult vaccinations provide information on older children and adults. Health Protection provides further information on infectious diseases and other noncommunicable health threats.
Vaccination coverage data can also be accessed via interactive dashboards:
2022/23 data published by NHS Digital shows that in Blackpool:
-
- The number of children who had received the 6-in-1 diphtheria, tetanus and pertussis (DtaP)/polio (IPV), haemophilus influenzae type b (Hib) and Hepatitis B vaccine at the age of 12 months was 1,517 (91.7%).
- The Men B vaccine, introduced in 2015, is offered at eight and sixteen weeks of age, with a booster on or after the first birthday. Men B coverage at 12 months in Blackpool was 1,511 (91.3%) children.
- The Rotavirus vaccine is offered at eight and twelve weeks of age, protecting against this highly infectious stomach virus. Rotavirus coverage at 12 months in Blackpool was 1,462 (88.3%).
- The number of children who had received the diphtheria, tetanus and pertussis (DtaP)/polio (IPV) and haemophilus influenzae type b (Hib) vaccine at the age 2 years was 1,547 (93.5%).
- The number of children who had received the Hib/meningitis C (MenC) booster by 2 years of age was 1,485 (89.8%).
- The number of children who had received the first dose of the measles, mumps and rubella (MMR) vaccine by 2 years of age was 1,496 (90.4%).
- The number of children who had received their Menigitis B (Men B) booster by 2 year of age was 1,464 (88.5%).
For infomation on older children see: Immunisations of children at age 5 years and over.
Figure 1: Percent of children immunised by their 1st birthday: 2022/23
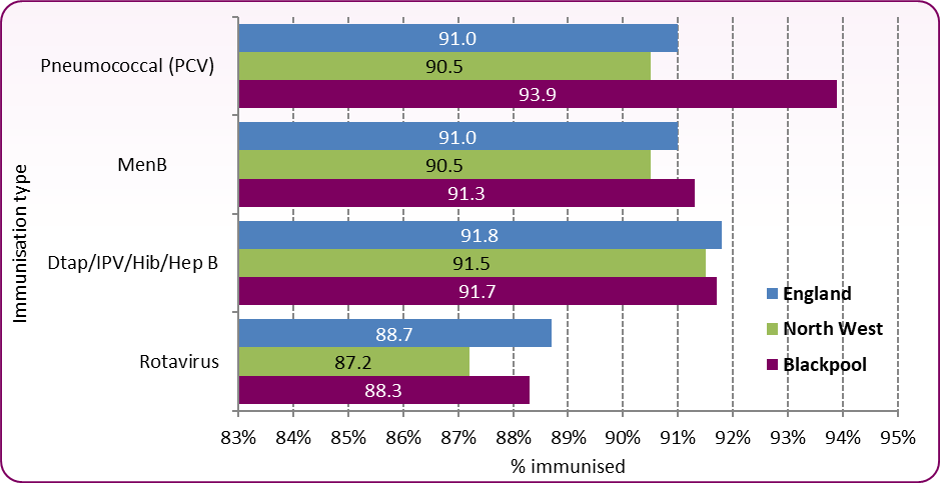 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Figure 2: Percent of children immunised by their 2nd birthday: 2022/23
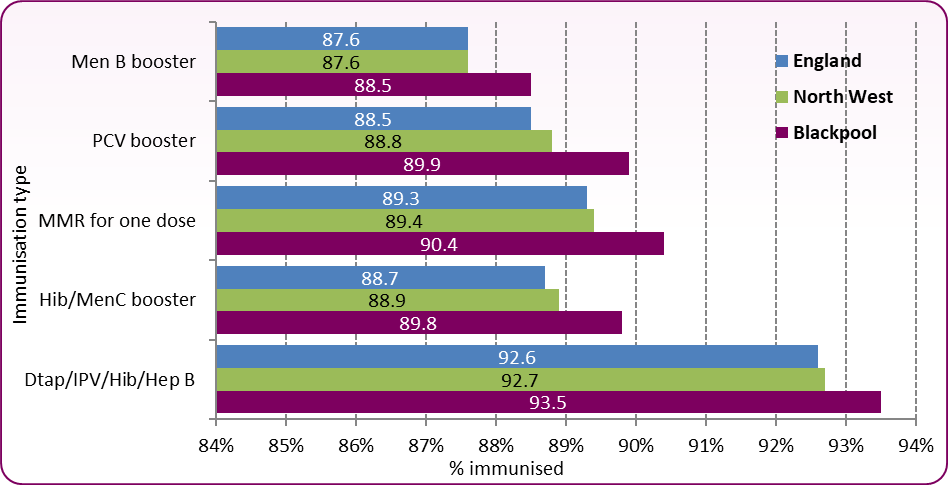 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Across Blackpool, immunisation uptake at the age of 1 year is slightly above the national average for PCV and MenB and slightly below the national average for DTap/IPV/Hib/HepB. However, all rates are now below the 95% uptake recommended by the World Health Organization (WHO) (Figure 1). Similarly, though rates of immunsation in 2 year old children are above national averages (Figure 2), they are below the 95% recommended uptake and uptake continues the decreasing trend of the last few years (Figure 3 and Figure 4).
Vaccination coverage is the best indicator of the level of protection a population will have against vaccine preventable communicable diseases. Coverage is closely correlated with levels of disease and monitoring coverage identifies possible drops in immunity before levels of disease rise.
Figure 3: Trend in vaccination coverage, children aged 2 years (%)
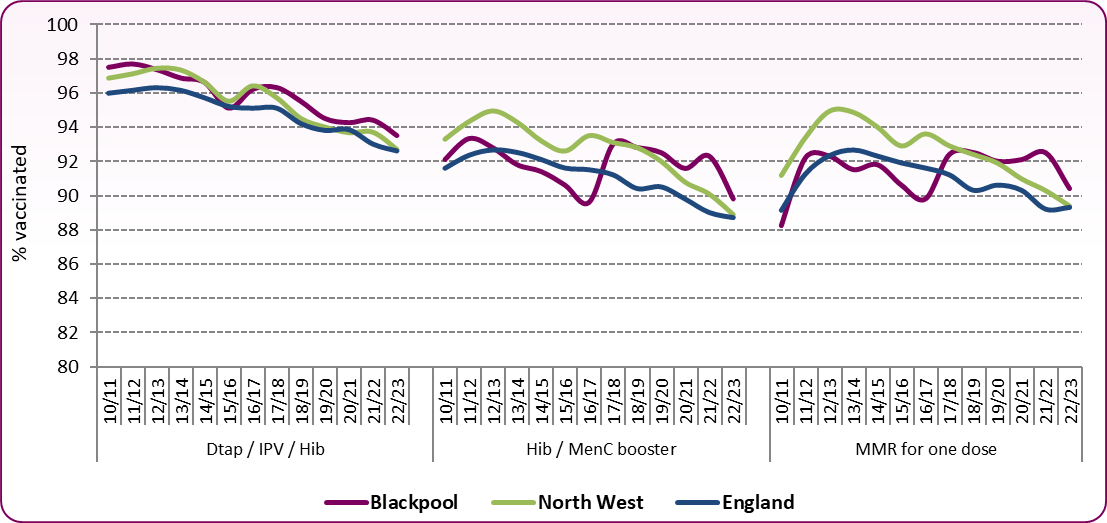 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
Figure 4: Trend in uptake of MMR vaccine, children aged 2 years (%)
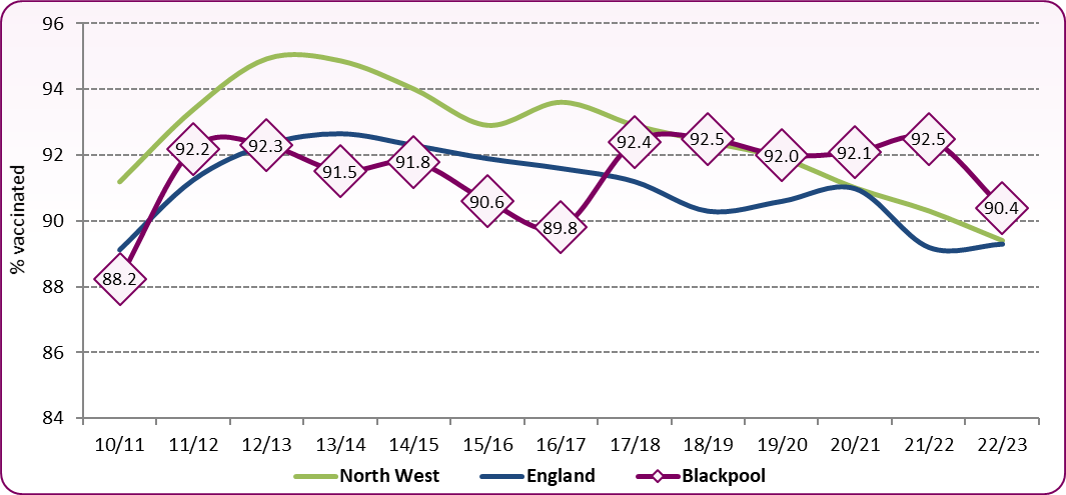 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
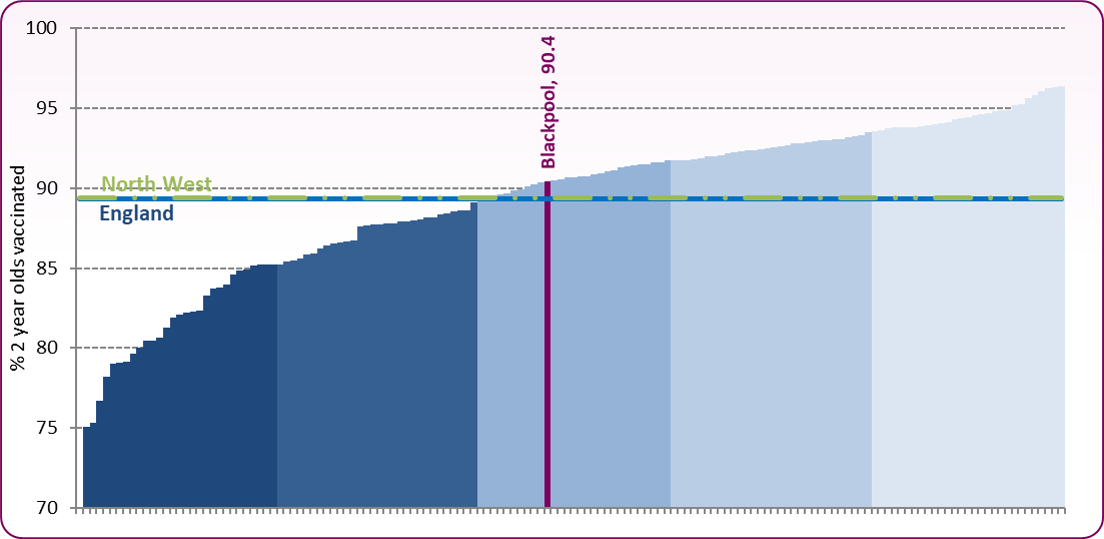
Despite maintaining a rate above the national average since 2017 (Figure 4), MMR coverage in Blackpool and across England remains below the WHO target of 'at least 95%' coverage and 2022/23 saw a sharp drop after a few years of stable uptake. The spike in coverage in 2010/11 was due to a 'catch up' campaign. Figure 5 shows Blackpool compared with other local authorities in the country. With a 2022/23 coverage rate of 90.4%, Blackpool is ranked 79/149 of upper tier local authorities and is in the third (middle) quintile.
Figure 5: Population vaccination coverage - MMR for one dose (2 years old), upper tier local authorities, 2022/23
 Source: OHID, Health Protection Profile
Source: OHID, Health Protection Profile
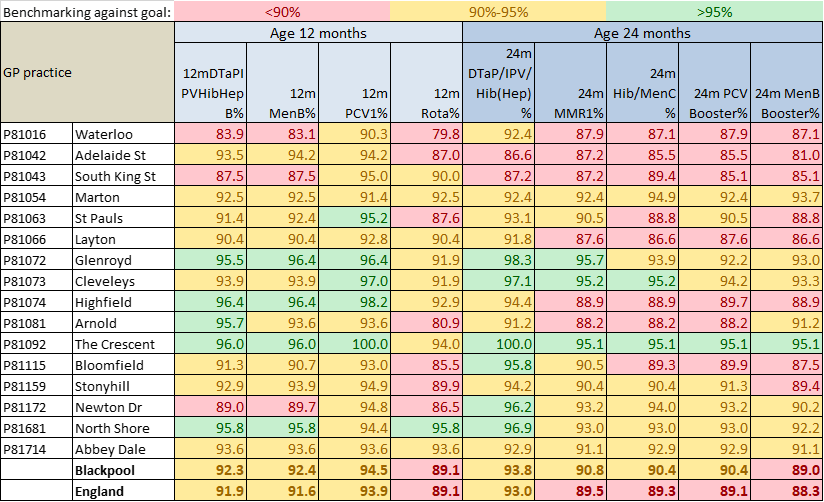
At a local level, there is variation in the proportion of children immunised in each of Blackpool's GP practices. Figure 6 shows immunisations due at age 1 year and at age 2 years and the proportion of children immunised by each practice in 2022/23.
Figure 6: Child Immunisations by GP Practice in Blackpool, 2022/23
 Source: UKHSA, Cover of vaccination evaluated rapidly (COVER) programme 2022 to 2023: quarterly data
Source: UKHSA, Cover of vaccination evaluated rapidly (COVER) programme 2022 to 2023: quarterly data
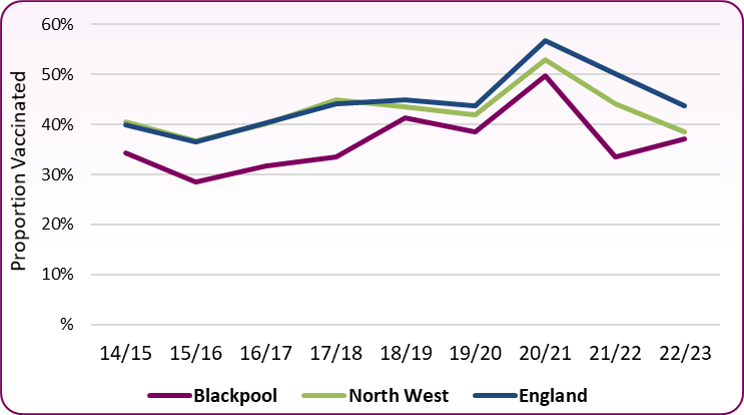
Influenza
In 2012 the Joint Committee on Vaccination and Immunisation (JCVI) recommended that the Influenza programme be extended to all children aged two to less than 17 years. A phased introduction of the influenza programme began in 2013, with a national ambition in 2021/22 to achieve at least 70% vaccine uptake in those aged 2 to 3 years old. Rates continued to rise, reaching a high of 49.7% in Blackpool in 2020/21. In line with the national picture, rates fell in 2021/22 (Figure 8) but 2022/23 has seen an increase with 37.1% vaccinated in Blackpool. Although nationally, rates fell again in 2022/23 to 43.7%, Blackpool still has significantly lower uptake rates.
Figure 8: Trend in Influenza Vaccination Coverage (2-3 year olds), Blackpool, North West and England, 2014/15 to 2022/23 Flu Seasons
 Source: OHID Health Protection Profile, Immunisation and childhood vaccination preventable diseases
Source: OHID Health Protection Profile, Immunisation and childhood vaccination preventable diseases
There are many reasons why people choose not to immunise themselves or their children. Studies have looked into how parents make decisions on whether to vaccinate their children or not and found that this is related to gaps in their knowledge of vaccine preventable diseases, concerns over vaccine safety and their attitudes towards immunisations, health professionals and health organisations.
Blackpool recognises that there is a need to target both overall improvement of immunisation coverage and specifically to improve the low levels of coverage amongst certain groups and in certain places.
Evidence has shown that the groups of children and young people who are most at risk of not being fully immunised are2:
• those who have missed previous vaccinations (as a result of parental choice or otherwise)
• looked after children
• those with physical or learning disabilities
• children of teenage or lone parents
• those not registered with a GP
• younger children from large families
• children who are hospitalised or have a chronic illness
• those from some minority ethnic groups
• those from non-English speaking families
• vulnerable children, such as those whose families are Gypsy Travellers, asylum seekers or are homeless.
[] WHO Regional Office for Europe, European Immunization Agenda 2030, 2021
[] NICE, [PH21] Reducing differences in the uptake of immunisations (including targeted vaccines) among children and young people aged under 19 years. London: National Institute for Health and Clinical Excellence; September 2017