Suicide
Last Modified 29/02/2024 12:24:05
Share this page
Introduction
In September 2023 the Government released Suicide prevention in England: 5-year cross-sector strategy aiming to reduce the number of lives lost to suicide.
While all areas of the country now have local suicide prevention plans and suicide bereavement services in place and the overall current suicide rate is not significantly higher than in 2012, the rate is not falling. The aim of this cross-government strategy is to bring everybody together around common priorities and set out actions that can be taken to:
-
-
-
reduce the suicide rate over the next 5 years – with initial reductions observed within half this time or sooner
-
improve support for people who have self-harmed
-
improve support for people bereaved by suicide
Suicide remains a major public health issue as Blackpool continues to have one of the highest suicide rates in the country, with a rising trend in female suicide; steps need to be taken to reduce the number of suicides locally.
Facts and figures
Deaths from suicide in England in 2022 was similar to the previous year, 5,284 compared to 5,219 in 2021. The rate of 10.3 per 100,000 pop. was just slightly lower than the previous year, 10.4 per 100,000.1 Figures for Blackpool show:
-
-
Blackpool had the sixth highest rate of suicide of any upper tier local authority in England, for all persons (aged 10 years and over), during the period 2020-22 (figure 1)
-
Blackpool has a significantly higher suicide rate (16.4 per 100,000 population) than England as a whole (10.3)
-
There were 61 deaths from suicide and undetermined injury in the three-year period 2020-22
-
66% (40) were male, 34% (21) were female.
Figure 1: Mortality from suicide and injury undetermined, upper-tier local authorities, 2020-22 (persons aged over 10)
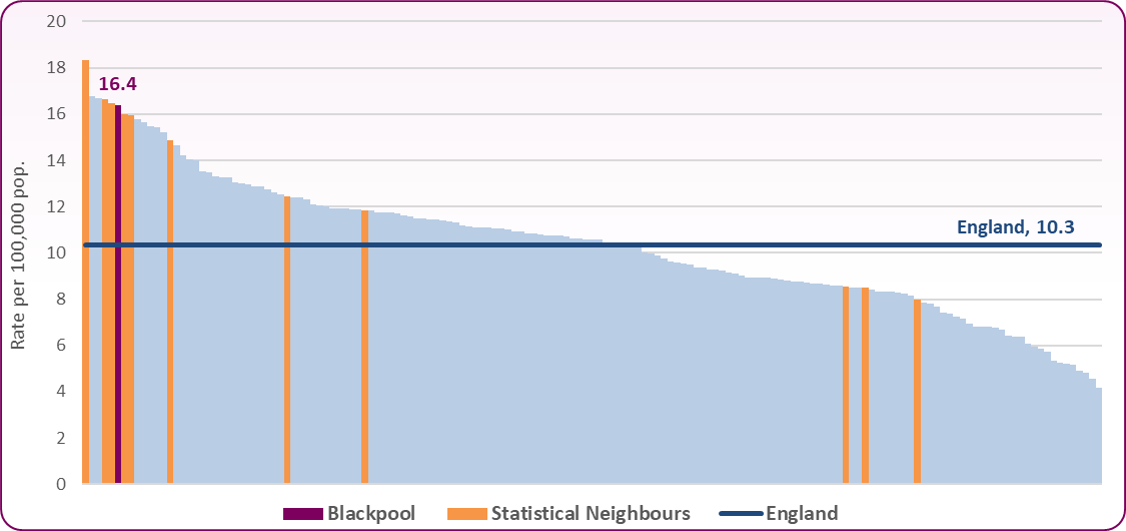 Source: OHID, Suicide Prevention Profile
Source: OHID, Suicide Prevention Profile
Figure 2 shows there is a significant difference in the number of suicides between the sexes in Blackpool, the North West and England. Mortality from suicide and undetermined injury is three times higher in males compared to females in England and the North West. Blackpool however has an increasing trend in female suicides (figure 3) and the rate is now half the male suicide rate.
Figure 2: Mortality from suicide and injury undetermined, males, females and persons, 2020-22
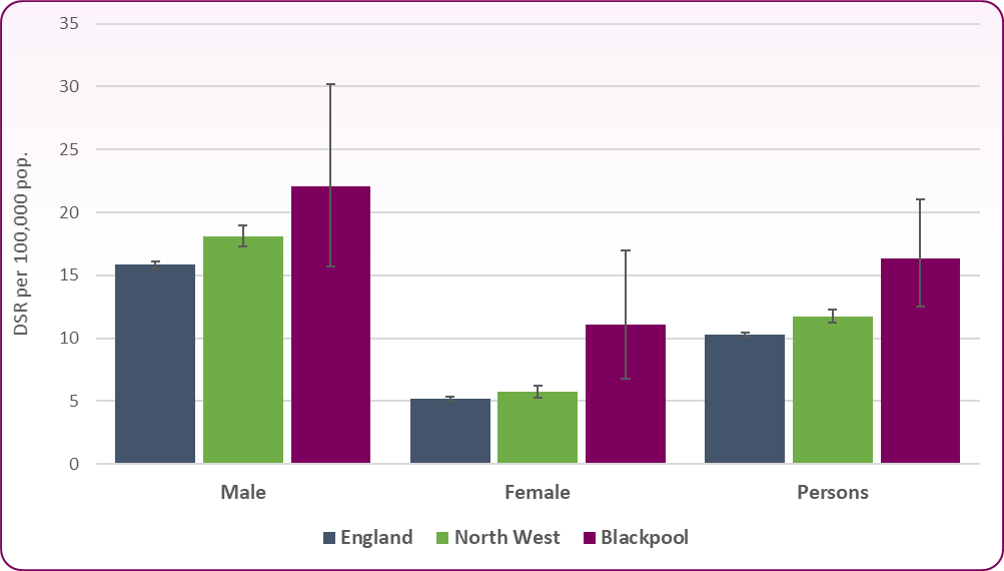 Source: OHID, Suicide Prevention Profiles
Source: OHID, Suicide Prevention Profiles
Figure 3: Trend in FEMALE suicide rate, Blackpool and England: 2001-03 to 2020-22
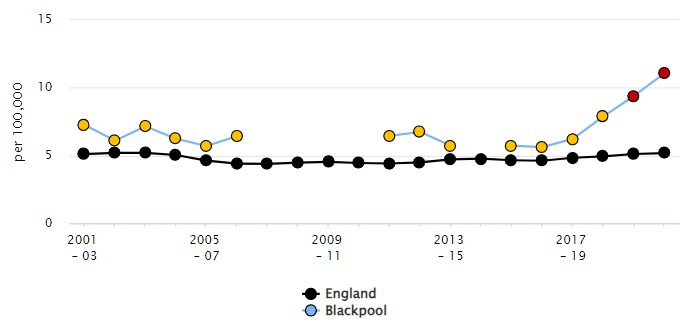 Source: OHID, Suicide Prevention Profile
Source: OHID, Suicide Prevention Profile
The most common age of suicide in Blackpool was between 45-54 years, with over a quarter (28%) of deaths in this age group. Just under a fifth were aged over 65 and less than 10% were aged under 25 years.
Figure 4 shows the overall trend in the mortality rate from suicide in Blackpool, the North West and England. Apart from in 2009-11, Blackpool has remained significantly higher than England as a whole over the 20 year period.
Figure 4: Trend in mortality from suicide and injury undetermined, 2001-03 to 2020-22 (persons aged over 10)
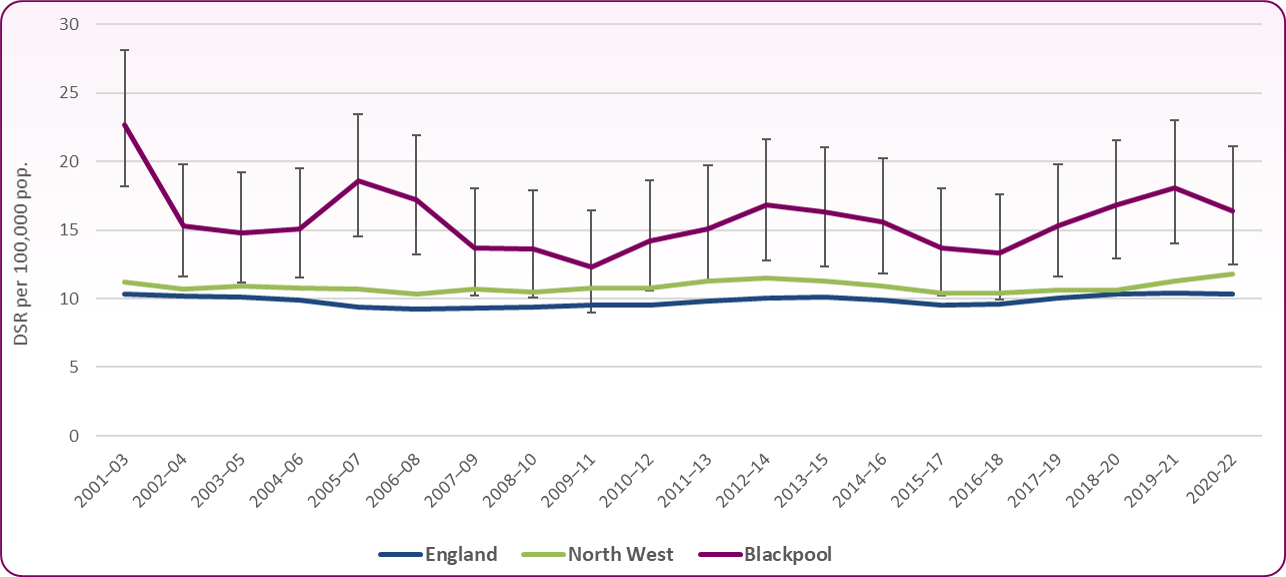 Source: ONS, Suicides in England and Wales: 2022 registrations, December 2023
Source: ONS, Suicides in England and Wales: 2022 registrations, December 2023
Blackpool Suicide Audit 2015 - executive summary
Public health completed a suicide audit using data collected from the coroner's office, primary care records, secondary care records and custody. Due to relatively small numbers the audit is completed by pooling data over the three year period, 2011-13. Results from the audit found:-
-
-
There were 55 deaths registered in 2011-13. For the purposes of the report only 50 deaths were audited due to a number of case files being unavailable.
-
74% (37) of deaths by suicide in 2011-13 were male, and the most common age recorded at time of death was 25-44 years.
-
26% (13) of deaths by suicide in 2011-2013 were female and the most common age recorded at time of deaths was 40-59 years
-
Half of females (6/13) die from suicide in the month between December and January (6), the highest frequency of suicides in males occurred between May-July (21/31)
-
Analysis of suicides by geo-demographic type (Mosaic) showed the highest number of suicides in categories L49 (disconnected youth), O63 (streetwise single), L52 (midlife stopgap), K46 (self-supporters) and L50 (renting a room).
-
The most common method of suicide in males is hanging/strangulation with (52%)
-
Over half (64%) of those who died by suicide did so at home.
-
A history of depression, mental illness, history of drug and alcohol abuse, self-harm, having a long term condition and alcohol use present as high risk factors for suicide. Being unemployed, single, living alone, having financial and relationship difficulties also feature strongly as co-existing factors.
-
Depression was the most common current and/or ongoing mental health diagnosis with 54% of females and 40% of males recorded as having depression in 2011-13.
-
Nearly half of all suicides (46%) in contact with primary care beforehand had been prescribed medication by their GP.
-
22% (11) of suicides had a history of alcohol/drug misuse recorded in either the coroner's records or their primary care notes.
-
Nearly half of all suicides (46%) had been in contact with primary care in the last month.
-
12% had contact with a health care professional (usually the GP) in the week before death, and 24% in the month before death.
-
28% (14) of suicides had been in contact with specialist mental health services in their lifetime.
-
35% (13) of all male suicides and 38% of all women (5) were reported to have had either a lifetime history of self-harm or within the last 12 months of their lives.
Ambulance callouts relating to psychiatric problems and/or suicide
Data from Safer Lancashire shows Blackpool has the highest ambulance incidence rate for psychiatric/suicide attempts in the Lancashire-14 area.2 There were 772 callouts for psychiatric/suicide attempts in Blackpool, out of 3,862 for the same across Lancashire-14 (2022/23).
-
-
Blackpool's ambulance incidence rate for psychiatric/suicide issues (5.5 per 1,000 persons) is over twice the Lancashire-14 rate (2.5) (2022/23)
-
Incidents showed a decrease in Blackpool from a high of 9.4 in 2016/17 to 3.7 in 2020/21, although this is starting to rise again (figure 5)
Figure 5: Trend in ambulance incidence rates for psychiatric/suicide issues, Blackpool and Lancashire-14, 2012/13 to 2022/23
 Source: Safer Lancashire MADE
Source: Safer Lancashire MADE
Risk factors
Suicide is a complex event, with rarely one significant contributing factor, and sometimes occurs for reasons that are not clear. Certain factors are known to be associated with increased risk. The national strategy3 identifies the following higher risk groups:
-
- children and young people
- middle-aged men
- people who have self-harmed
- people in contact with mental health services
- people in contact with the justice system
- autistic people
- pregnant women and new mothers
Common risk factors linked to suicide are:
-
- physical illness
- financial difficulty and economic adversity
- gambling
- alcohol and drug misuse
- social isolation and loneliness
- domestic abuse
Analysis by Office for National Statistics4 found that men are at least three times as vulnerable to death from suicide as women. This greater risk is suggested to be due to a complex set of reasons, including increased family breakdown leaving more men living alone; the decline of many traditionally male-dominated industries; and social expectations about masculinity.
Relationship breakdown can also contribute to suicide risk. The greatest risk is among divorced men, who in 2015 were almost three times more likely to end their lives than men who were married or in a civil partnership.
People who live in more deprived areas - where there is less access to things like services, work and education - are also more at risk of suicide; people among the most deprived 10% of society are more than twice as likely to die from suicide than the least deprived 10% of society.
A report by the Royal College of Psychiatrists stated that self‑harm is one of strongest predictors of suicide, including among older people and suicide occurs more frequently with the coexistence of psychiatric and physical illness.5
National and local strategies
Suicide prevention in England: 5-year cross-sector strategy (September 2023) aims to bring everybody together around common priorities and set out actions that can be taken to:
-
- reduce the suicide rate over the next 5 years – with initial reductions observed within half this time or sooner
- improve support for people who have self-harmed
- improve support for people bereaved by suicide
PHE, Public Health matters - keeping our focus on suicide prevention (Jan 2017) is a resource to support local areas in their work to save lives.
PHE, Local suicide prevention planning: A practice resource (September 2020) is a resource to support local authority public health teams to work with sustainability and transformation partnerships (STPs) and integrated care systems (ICSs), health and wellbeing boards, the voluntary sector and wider networks of partners to implement local suicide prevention plans and embed work within local sustainability and transformation plans.
PHE, Preventing suicides in public places, (November 2015) a practice resource is for those with responsibility for suicide prevention in local authorities and their partner agencies.
Recommendations
1) Ensure that all those working with high risk groups continue to have access to Applied Suicide Intervention Skills Training (ASIST) on suicide prevention, including those working in schools and colleges, emergency departments, other emergency services, primary care, care environments and the criminal and youth justice systems.
-
-
-
To ensure that staff of housing associations, job centres, and GPs that come into contact with individuals in distress as a result of benefit changes and other types of economic loss, know where to signpost individuals to appropriate support services and are ASIST trained.
2) Develop specific interventions for men aged 25 - 55 years to improve the mental health, resilience and access to support.
-
-
-
When developing interventions these should be done in collaboration with the men they are designed for.
-
Target campaigns and take services to where men are such as workplaces, online, pubs, sports grounds, betting shops, prisons etc.
-
When commissioning suicide prevention activities particularly targeting adult men aged under the age of 50 years, attention needs to focused on 'out of hours' services and the workplace.
-
Offer a range of support to individuals presenting in primary care including signposting for social support, such as housing, debt advice, bereavement and relationship difficulties, social prescribing and 'talking therapies'.
-
Use mosaic profiles to target suicide prevention activities e.g. social marketing messages.
3) In light of the connection between drug and alcohol and mental health issues, an integrated approach to suicide prevention strategies for this cohort would provide more robust interventions.
-
-
Local substance misuse agencies should ensure that all are competent to assess the risk and prevent suicide among individuals who are most vulnerable.
-
Mental health and substance misuse workers to develop and facilitate joint working protocols.
-
Assertive outreach teams in both mental health and substance misuse services to prevent loss of contact with vulnerable and high risk patients.
-
Depression screening for elevated suicide risk for those admitted with alcohol/drug dependence in primary/secondary care.
4) Review care pathways for people in contact with accident & emergency, drug and alcohol services and North West Ambulance Service (NWAS) who present with deliberate self-harm, with the aim to address the assessment of suicide risk, mental health needs and substance misuse.
5) Explore piloting 'real-time' surveillance of suicides in collaboration with the police, who are usually first on the scene of suicide deaths. The primary aim of the pilot is to provide information to front line local authority and NHS staff to enable them to respond to local clusters of suicides and to improve access and provide timely support to people bereaved by suicide.
6) Pilot local GPs to provide public health with 'real time' significant event questionnaire.
7) Explore the development of a 'flag system' within primary care for frequent attenders to their GP.
8) Invest in and support campaigns to reduce loneliness and social isolation particularly targeting men who are in contact with drug and alcohol services.
9) Public health to review the process for future audits including the revision of the audit toolkit.
10) Work with Blackpool Council and the integrated care system's marketing and communications team to encourage local media to report stories around suicide and self-harm responsibly and to provide information about sources of support and helplines when reporting suicide and suicidal behaviour.
11) Work with planning departments and developers to include suicide in health and safety considerations when designing structures which may offer suicide opportunities. Also work with neighbourhood services to designing and maintaining suicide prevention signage, particularly at hot spots.
[] Office for Health Improvement and Disparities, Suicide Prevention Profile
[] Safer Lancashire Multi-Agencey Data Exchange (MADE): MMIR and District Profile 15.1 http://www.saferlancashire.co.uk/2011/
[] DHSC, Policy paper, Suicide prevention in England: 5-year cross-sector strategy, September 2023
[] ONS, Who is most at risk of suicide? Analysis and explanation of the contributory risks of suicide. September 2017
[] Self-harm and suicide in adults: Final report of the Patient Safety Group, Royal College of Psychiatrists, July 2020