Cancer
Last Modified 29/11/2023 09:39:52
Share this page
Introduction
Cancer occurs when abnormal cells within the body divide in an uncontrolled way. Some cancers may eventually spread into other tissues. Most cancers start due to gene changes that happen over a person's lifetime, with certain lifestyle and environmental factors increasing the risk of developing cancer. More rarely cancers start due to inherited faulty genes passed down in families.
Cancer is a common condition and one in two people living in the UK will develop the disease at some point in their lifetime. Over 250,000 people in England are diagnosed with cancer every year and around 130,000 die from the disease. Currently, in England, about 2.2 million people are living with a cancer diagnosis, with 7,093 of these people registered to a Blackpool GP practice. Even if an individual does not develop cancer, it is likely their friends and family will have it. Surveys show that people fear cancer more than anything else.1
Facts and figures
Incidence of cancer
Incidence is defined as the number of new cases identified in a given period of time.
In Blackpool each year there are between 860 and 1,050 new cases of cancer identified (888 in 2020). Figure 1 shows the trend in the cancer incidence rate in Blackpool and England. The incidence rate (in this case per 100,000 population) is calculated to allow comparison between geographies of different population sizes and with different gender and age make ups.
Across England, cancer incidence rose slightly through the 2000s, but this trend stopped around 2013. Cancer incidence in Blackpool has remained consistently higher than that seen nationally, with rises in both male and female incidence between 2017 and 2019, although this has dropped off. It is likely that the COVID-19 pandemic meant people were less likely to contact a health professional with cancer symptoms, and this may have contributed to the reduced incidence.
Figure 1 - incidence of all malignant cancers (all ages) excluding non-melanoma skin cancer (NMSC)* - 2001-2020 annual trend
 Source: National Cancer Registration and Analysis Service (NCRAS), CancerData (www.cancerdata.nhs.uk) *cases of non-melanoma skin cancer (NMSC) have been inconsistently recorded over time and geography. Consistent comparisons over time and geography are made by excluding NMSC from trend data.
Source: National Cancer Registration and Analysis Service (NCRAS), CancerData (www.cancerdata.nhs.uk) *cases of non-melanoma skin cancer (NMSC) have been inconsistently recorded over time and geography. Consistent comparisons over time and geography are made by excluding NMSC from trend data.
The report Cancer and equality: key metrics 2015 (Public Health England, 2015) states that, in England:
-
- For most cancers, males have higher incidence rates than females. This is in part expected with certain lifestyle and environmental exposure causes of cancer, such as smoking and asbestos exposure also being higher in males. Cancers of the bladder, oesophagus, stomach and liver all had incidence rates more than twice as high in men than women.
- Inequalities in cancer incidence in relation to socio-economic deprivation are one of the major concerns. Incidence rates for cancers of the lung, larynx, liver (in males) and oral cavity (in males) are at least double in the most deprived groups compared to the least deprived. Incidence rates were also significantly higher in the most deprived groups for cancers of the oropharynx, oral cavity (females), oesophagus, stomach, pancreas, colorectal (in males), anus, vulva, cervix, penis, kidney, bladder, Hodgkin lymphoma (males), non-Hodgkin lymphoma (females) and acute myeloid leukaemia in males.
Prevalence of cancer
Prevalence refers to the number of people who have previously received a diagnosis of cancer and who are still alive at a given time. This reflects both the incidence of cancer and its associated survival pattern. High prevalence indicates high incidence and/or long survival, whereas low prevalence indicates low incidence and/or short survival.
Overall the Blackpool sub-location (formerly NHS Blackpool Clinical Commissioning Group) has a higher recorded prevalence of cancer compared with the national picture. During 2021/22, there were 7,093 people registered with Blackpool GP practices with a diagnosis of cancer. This is a prevalence rate of 4.0%, significantly higher than the national prevalence rate of 3.3%.2
Mortality from cancer
Whilst the overall incidence rate of cancer has increased nationally, the rate of people dying from cancer has decreased.
Each year in Blackpool there are approximately 460 deaths from cancer, which usually accounts for around a quarter of all deaths in the area. In 2021, there were 493 deaths (all ages, all people). The directly standardised mortality rate (in this case per 100,000 population) is calculated to allow comparison between geographies of different population sizes and with different gender and age make ups. Overall, mortality rates for cancers are significantly higher in Blackpool compared to the regional and national figures. The most common causes of death from cancer in Blackpool are lung, bowel and breast cancer.
Based on Office for National Statistics annual mortality extracts (for 2021 only) lung cancer accounts for a greater proportion of cancer deaths in Blackpool compared to England amongst people of all ages (24.5% compared to 19.4%) and for under-75s (29.7% compared to 21.3%).
Just over half of cancer deaths occur in people aged under-75 in Blackpool (52.5%) compared to 44.4% in England. Amongst the under-75s, mortality rates from cancer are around 50% higher in Blackpool compared with the national average. Please note, the three-year (2018-2020) mortality funnel chart and the annual trend chart below cannot be updated to incorporate more recent data at present. This is due to the revised official population estimates (based on the Census 2021) not being available to recreate the mortality trends. Once these are published, the charts will be updated.
Figure 2 - mortality from all cancers aged under-75 - 2018-2020 - lower tier local authorities3
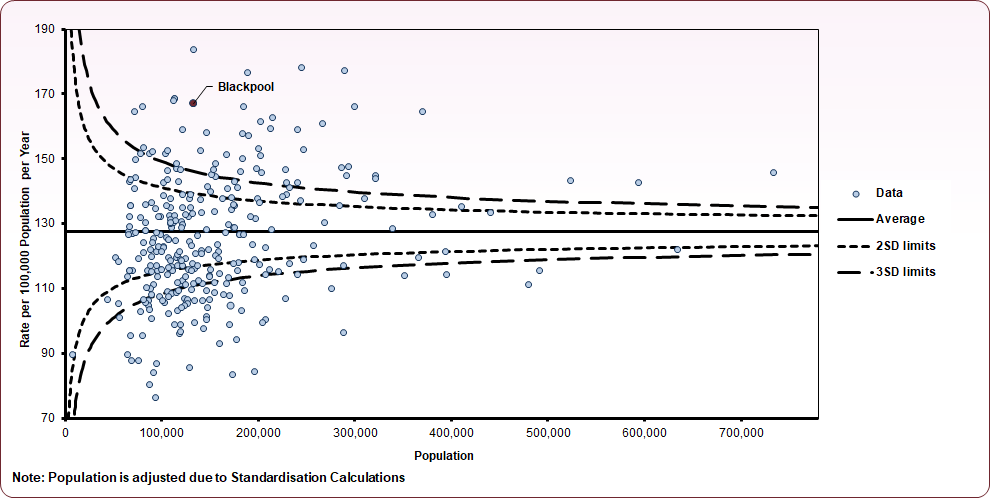 Source: NHS Digital, Compendium of Population Health Indicators
Source: NHS Digital, Compendium of Population Health Indicators
Over the last 25 years, cancer mortality rates amongst under-75s have shown an overall improvement, however the mortality rate in Blackpool has remained consistently higher than seen nationally and in the north west. Despite a reducing national rate, under-75 mortality from cancer has remained relatively steady in Blackpool from mid- to late 2000s onwards, with a decline in the male mortality rate since 2016 off-set by an increase in the female rate (figure 3).
Figure 3 - trend in cancer mortality (aged under-75), 1995-2020
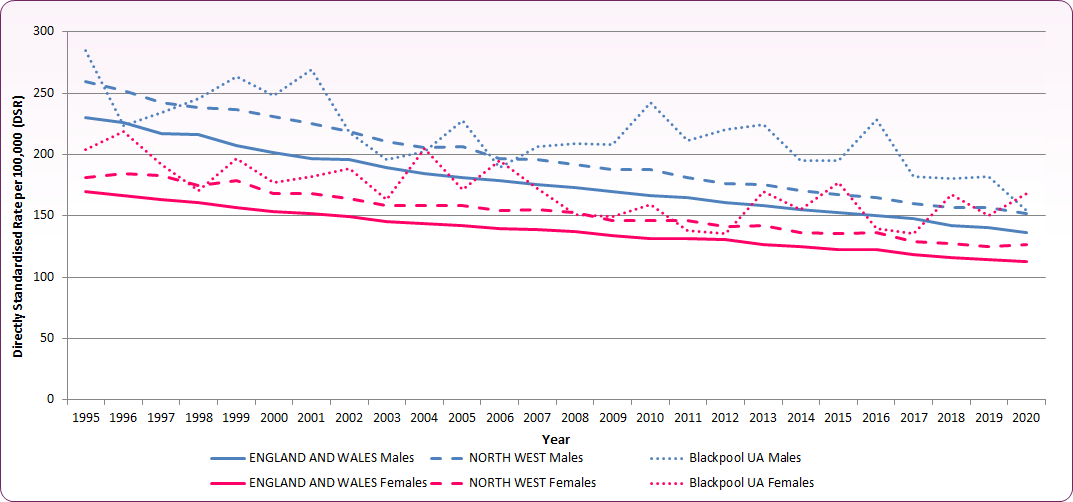 Source: NHS Digital, Compendium of Population Health Indicators
Source: NHS Digital, Compendium of Population Health Indicators
The report Cancer and equality: key metrics 2015 (Public Health England, 2015) states that, in England:
- Deaths from the four most common cancers account for 45% of all cancer deaths.
- For the majority of cancer types, males have higher cancer mortality rates than females. For bladder and oesophageal cancers, mortality rates were more than two and a half times higher for males, and for all cancers combined (excluding non-melanoma skin cancer, breast, lung and sex specific cancers) mortality rates for males are around 70% higher than females.
- As for cancer incidence, mortality rates for most cancers are significantly higher amongst the most deprived groups compared to the least deprived.
Cancer survival
Cancer survival rates give an indication of successful service provision, and variations could indicate practice that may need to be investigated further.
One-year cancer survival is defined as the proportion of individuals that survive for a year after diagnosis. The most recent data (2020) show the one-year cancer survival was 71.3% for individuals registered in Blackpool's sub-location (formerly NHS Blackpool Clinical Commissioning Group), compared to the England average of 74.6%. This survival rate is the fifth lowest in the country. One-year cancer survival for Blackpool patients has, however, improved significantly, rising from 61.1% in 2005 in line with increases seen nationally.
The report Cancer and equality: key metrics 2015 (Public Health England, 2015) states that, in England:
-
- Relative survival by age highlights the poorer relative survival rates for older cancer patients. For the four main cancers, those aged over 75 have significantly poorer survival rates than younger age groups.
- Survival is higher for females than males with lung cancer and melanoma. Male colorectal cancer patients have better survival rates than females.
- Residents of more deprived areas have worse survival for colorectal, lung and ovarian cancer.
Summary of cancer incidence, mortality and survival in Blackpool
Table 1 shows the most common types of cancer and summarises incidence, mortality and survival rates using directly standardised rates per 100,000 resident population2
Table 1: summary of cancer incidence, mortality and survival in Blackpool
| | Incidence - all ages | Mortality - age under-75 | Mortality - all ages | 1-year survival |
|---|
| | (2018-20) | (2018-20) | (2018-20) | (2020) |
|---|
| Breast (females only) |
142.1+
|
21.86 |
34.27 |
96.7% |
|---|
| Lung |
108.7* |
41.09* |
74.95* |
43.6% |
|---|
| Prostate (males only) |
135.9+ |
12.45 |
45.1 |
-- |
|---|
| Colorectal |
70.8 |
17.15* |
31.96 |
73.1% |
|---|
| Cervical (females only) |
13.6 |
4.32 |
3.93 |
-- |
|---|
*denotes value is significantly higher than England average; + denotes significantly lower than national average, -- Local data is not available for prostate and cervical cancers.Sources: Cancer survival: Index for sub-Integrated Care Boards, 2005 to 2020 - NHS Digital. CancerData
Cancer and equality
The report Cancer and equality: key metrics 2015 explores where there are differences between groups in aspects of cancer patients' diagnosis, care and outcomes. The report states that, in England:
-
- Inequalities in cancer incidence in relation to socioeconomic deprivation are one of the major concerns.
- Cancer mortality in the most deprived populations is 50% higher than in the least deprived.
- Emergency presentations, a marker of late diagnosis and worse prognosis, increases with age and has a clear socioeconomic gradient that worsens with deprivation.
- Patient surveys consistently identify a need for easier to understand information for patients across all age groups, and especially amongst younger cancer patients.
- Patient reported outcomes measures show socioeconomic gradient with poorer outcomes reported by more disadvantaged groups.
- For screening coverage, low rate of uptake of cervical screening amongst young women and the lower rates of uptake of colorectal screening in men are highlighted.
National and local strategies (current best practices)
Risk Factors
Risk factors for cancer broadly fall into three categories: genetic/hereditary, environmental, and lifestyle/behaviour risks. Cancer Research UK published work on the number of cancer cases in the UK that could be prevented by known lifestyle and environmental factors.4,5 The list below is taken from this work and lists factors which increase cancer risk, in order of relative magnitude:
-
- Tobacco - smoking any form of tobacco, or exposure to environmental tobacco smoke
- Overweight - having a BMI of 25 kg/m2 or over
- Radiation: UV (sunlight and sunbeds)
- Occupation - being exposed to cancer causing chemical or conditions at work
- Infections - exposure to cancer causing infections like HPV and hepatitis B or C
- Alcohol - drinking of any type of alcohol
- Insufficient dietary fibre - having less than 30 grams of fibre a day
- Radiation: ionising - being exposed to any ionising radiation, including background levels such as those released from the earth
- Eating processed meat
- Air pollution
- Not breastfeeding
- Inactivity - being moderately active for less than 120 minutes a week
- Postmenopausal hormones - taking hormone replacement therapy
- Oral contraceptives
Lifestyle factors associated with poorer health tend to reflect levels of relative disadvantage within the population.
Note: factors such as oral contraception may have a net protective effect against cancers. Cancer risks for HRT and oral contraceptives are considered to be relatively low and benefits may outweigh risks.6 If you have any concerns please speak to your GP.
Cancer, Britons most feared disease
Office for Health Improvement and Disparities, Cancer Services - OHID (phe.org.uk)
Note: five new local authorities have been omitted from the analysis due to concerns regarding data reliability.
Cancer Research UK, Statistics on preventable cancer
Brown KF, Rumgay H, Dunlop C, et al. The fraction of cancer attributable to known risk factors in England, Wales, Scotland, Northern Ireland, and the UK overall in 2015. British Journal of Cancer, 2018
Cancer Research UK, Does hormone replacement therapy (HRT) increase cancer risk?