Mental Health
Last Modified 05/02/2024 16:20:07
Share this page
Introduction
Mental health is defined by the World Health Organisation (WHO) as "a state of well-being in which every individual realises his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community." Mental health problems are among the most common forms of ill health. They can affect people at any point in their lives. Mental health and physical health are inextricably linked. Poor physical health may increase the likelihood of developing poor mental health, and poor mental health may increase risks of developing, or not recovering, from physical health problems.
Across England:
-
- 1 in 6 adults will have experienced a common mental health disorder in the past week
- severe mental illness such as schizophrenia or bipolar disorder affects around 550,000 people
- together with substance misuse, mental illness accounts for 21.3% of the total burden of disease across the country
- the costs of mental health problems to the economy in England have recently been estimated at £105 billion
- half of mental health problems have been established by the age of 14, rising to 75% by age 24
- those in the poorest fifth of the population are twice as likely to be at risk of developing mental health problems as those on an average income.1
The COVID-19 pandemic has also had an effect on the mental health of the UK population, with a general deterioration in mental health and wellbeing during lockdown periods. Some studies have shown gradual improvements towards pre-pandemic levels following lockdown easing, though these periods of 'recovery' were not observed in all studies, and self-reported mental health and wellbeing across the population remains worse than before the pandemic. The mental health effects of COVID-19 were different for different groups of people, and general population statistics may mask more profound impacts on these groups. Women, young adults, those with pre-existing mental health conditions, adults experiencing loss of income or employment, those living in deprived neighbourhoods, some ethnic minority populations, extraverted individuals and those living alone may have been more likely to experience worse or deteriorating mental health during this period.1,2
Facts and figures
Traditionally a distinction has been drawn between severe and enduring mental illness, and common mental health problems:
-
- Severe and enduring mental health problems include psychotic disorders (including schizophrenia) and bipolar affective disorder and other psychoses which affect a person's cognition, insight and perception
- Common mental health problems include problems such as anxiety, depression, phobias, obsessive compulsive and panic disorders.
- Personality disorder is defined as "an enduring pattern of inner experience and behaviours that deviates markedly from the expectation of the individual's culture, is pervasive and inflexible, has an onset in adolescence or early adulthood, is stable over time and leads to distress or impairment"
The organisation and delivery of services has been significantly influenced by this distinction between severe mental illness and other conditions. However, it is increasingly recognised that diagnosis alone is a poor indicator of severity, complexity, or disability in mental illness.
Figure 1 displays the number of people aged between 18 and 64 estimated to have a mental health disorder in Blackpool.
Figure 1 - Mental Health Disorders - Blackpool
| Mental health condition | 2023 | 2025 | 2030 | 2035 | 2040 |
|---|
| People aged 18-64 predicted to have a common mental disorder |
15,141 |
15,036 |
14,702 |
14,496 |
14,459 |
| People aged 18-64 predicted to have a borderline personality disorder |
1,923 |
1,909 |
1,867 |
1,841 |
1,836 |
| People aged 18-64 predicted to have an antisocial personality disorder |
2,693 |
2,670 |
2,617 |
2,590 |
2,583 |
| People aged 18-64 predicted to have psychotic disorder |
561 |
557 |
545 |
538 |
537 |
| People aged 18-64 predicted to have two or more psychiatric disorders |
5,773 |
5,731 |
5,607 |
5,534 |
5,520 |
| Source: Projecting Adult Needs and Service Information (PANSI) |
The Common Mental Health Disorders profile developed by the Office for Health Improvement & Disparities (OHID) illustrates that the prevalence of depression, both identified by GPs and self-reported within the GP patient survey, is significantly higher in Blackpool than the England average. In the 2023 GP Survey, 17.5% of Blackpool patients self-reported having a mental health condition.
Figure 2 shows Blackpool's 2022/23 prevalence of GP diagnosed depression is the highest in the country at 21.6% (up from 20.6% in 2021/22), significantly higher than the national average of 13.2%. There were 3,063 new diagnoses of depression recorded on GP practice disease registers in Blackpool in 2022/23, 2.1% of the GP registered population (18 years and over). This is similar to 2021/22 when the rate was 2.3%. Across England the rate of new diagnoses was 1.4% (1.5% in 2021/22).
Antidepressant prescribing levels have been rising steadily both nationally and locally, and NHS Lancashire and South Cumbria sub-integrated care board - 00R (formerly NHS Blackpool CCG) GP practices have some of the highest rates of prescribing antidepressants in England.3
In 2021/22, just under 2,800 Blackpool patients with schizophrenia, bipolar affective disorder and other psychoses were recorded on GP practice disease registers, 1.58% of the total registered GP population. The overall rate for England was 0.95%.
Figure 2: Diagnosed depression prevalence funnel plot analysis at sub-ICB (formerly CCG) level (2022/23 Quality and Outcomes Framework)
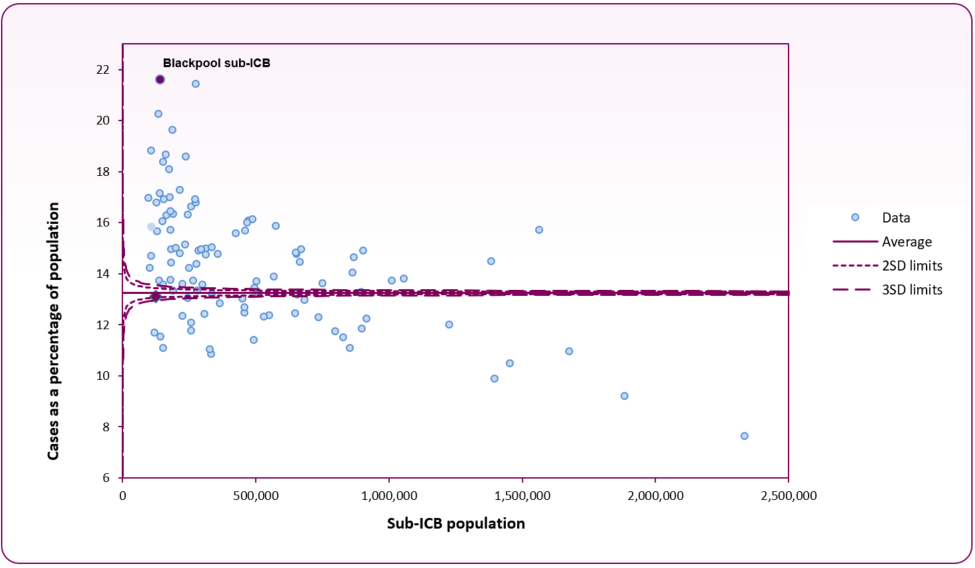 Source: OHID, Common Mental Health profile
Source: OHID, Common Mental Health profile
The OHID Mental Health and Wellbeing JSNA produce a range of wellbeing indicators. For Blackpool, the JSNA identified:
-
- 8.2% of people (16-years and over) had a low satisfaction score (self-reported wellbeing), significantly higher than England (5.0%) (2021/22)
- 8.0% of people (16-years and over) had a low worthwhile score, significantly higher than England (4.0%) (2021/22)
- 10.9% of people (16-years and over) had a low happiness score, statistically similar to England (8.4%) (2021/22)
- 23.7% of people (16-years and over) had a high anxiety score, statistically similar to England (22.6%) (2021/22)
Figure 3 - summary of Blackpool responses to wellbeing questions in the Annual Population Survey 2022-23
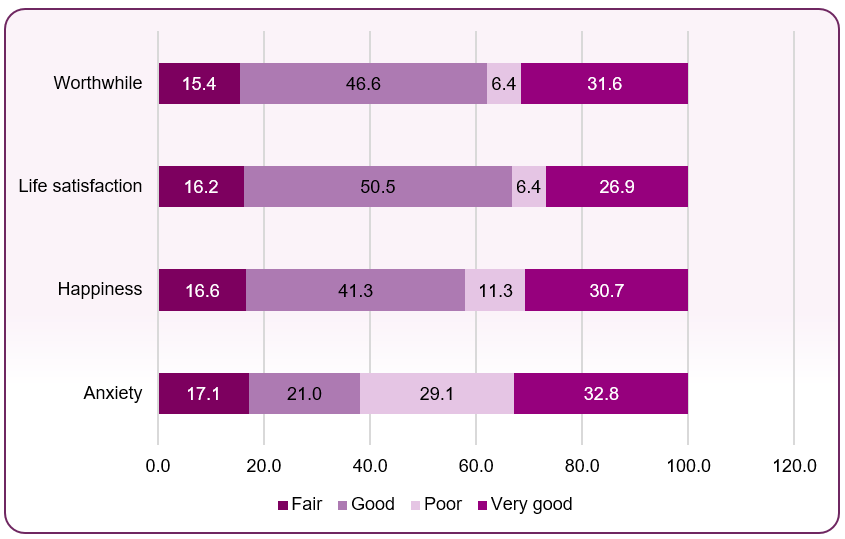 Source: ONS annual personal wellbeing estimates, 2022-23
Source: ONS annual personal wellbeing estimates, 2022-23
Views of the local community
Healthwatch Blackpool surveyed patients using community based adult mental health services provided by Blackpool Clinical Commissioning Group (CCG). Their report, Community Adult Mental Health report (December 2016) summarises the views of people using the service to provide a broader and clearer picture of service provision across the area.
National and local strategies (current best practices)
The government has developed a major conditions strategy. Rather than a stand-alone mental health strategy, mental ill health will be considered alongside other physical health conditions. A separate strategy for suicide and self-harm has also been produced.
Wellbeing and Mental Health: Applying All Our Health (PHE / Office for Health Improvement & Disparities, 2022 update) a resource which helps health professionals prevent ill health and care professionals use their trusted relationships with patients, families and communities to improve their mental wellbeing.
Advancing Mental Health Equalities Strategy (NHS England / NHS Improvement, 2020) identifies core actions to bridge the gaps for communities fairing worse than others in mental health services, particularly in the light of the impact of Covid-19.
NICE Common mental health problems: identification and pathways to care (CG123) covers care for people aged 18 and over.
Lethal Discrimination (Rethink Mental Illness, 2013) highlights why people with mental illness are dying early and needlessly and identifies what needs to change.
Closing the Gap: Priorities for essential change in mental health (Department of Health, 2014) identifies 25 aspects of mental health care and support where government – along with health and social care leaders, academics and a range of representative organisations – expect to see tangible changes.
Surviving or Thriving: The State of the UK's Mental Health (Mental Health Foundation, 2017) summarises the results of a national survey that aimed to understand the prevalence of self-reported mental health problems, levels of positive and negative mental health in the population, and the actions people take to deal with the stressors in their lives.
The Blackpool Public Mental Health Action Plan 2016-2019 used a public health approach to promoting mental wellbeing and preventing mental health problems. It incorporated interventions at both a universal level (to improve the mental health of our local population) and targeted level (targeting those groups and communities most at risk of poor mental health).
Advice and useful links are available from Blackpool Council’s mental health and wellbeing site.
Risk factors
'Fair Society Health Lives (Marmot Review)' identifies a number of factors that have a negative impact on mental health.These include:
-
- Being unemployed
- Being homeless
- Being poor
- Having a physical illness
- Having a drug or alcohol problem
Mental health, individual resilience and social exclusion are influenced by a range and interaction of different factors across the life course such as social position, education, housing, employment and exposure to crime or violence. The Marmot Report of 2010 described the role of addressing the wider determinants of health in improving health and reducing inequalities,and the contribution of positive mental wellbeing to preventing mental illness.
There are higher levels of substance misuse amongst people with psychosis. Approximately 40% of people with psychosis are reported to have misused substances at some point in their life and this is around double the rate seen in the general population.
[] Office for Health Improvement & Disparities (OHID) (2022 update) Wellbeing and Mental Health: Applying All Our Health
Office for Health Improvement & Disparities (OHID) (2022) COVID-19 Mental Health and Wellbeing Surveillance: Report
Office for Health Improvement & Disparities (OHID), Common Mental Health Disorders Profile