Breastfeeding
Last Modified 08/01/2024 12:57:34
Share this page
Introduction
Breastfeeding is good for babies and is recommended for about the first 6 months of a baby's life. Breasfeeding alongside solid foods is best for babies from 6 months. Not only does breastfeeding help build a strong emotional bond between mother and baby, the health benefits of breastfeeding babies are considered to be; reduced chance of diarrhoea and vomiting, fewer chest and ear infections, not as much chance of being constipated or developing eczema and less likelihood of becoming obese. The health benefits of breastfeeding for mothers are lower risks of developing certain ovarian and breast cancers, osteoporosis, cardiovascular disease and obesity1.
Analysis carried out by the Office for Health Improvement and Disparities (OHID) also indicates that higher rates of breastfeeding are associated with lower rates of obesity and overweight in children and mothers. Those areas with higher rates of breastfeeding at 6-8 weeks are seen to have slightly lower rates of obesity in children at age 4-5.2
Facts and Figures
Breastfeeding data focuses on two main areas: the initiation of breastfeeding, or first feed of breastmilk, and whether breastfeeding has been maintained after six to eight weeks. Both of these measures have undergone changes over recent years, and some data may be less reliable due to these changes and the challenge of obtaining a reliable level of completed data. Because of these factors, trend data should be read with caution.
Breastfeeding Initiation / First Feed
Figure 1 measures the percentage of newborn babies who commence breastfeeding. Until the end of 2016/17 this was measured by whether the mother gave their baby breastmilk within the first 48 hours after delivery. The new measure from 2020/21 is the proportion of babies whose first feed is known to be breast milk.
The chart compares the proportion of babies whose first feed is breast milk across local authorities in the North West. The new measurement for 2020/21 shows most local authorities in the north west have significantly lower breast feeding rates than the England average of 71.7%. Only Trafford and Cheshire East have rates significantly higher than this. Blackpool's rate is significantly lower than the England average, with 690 babies in 2020/21 receiving breast milk as their first feed, a rate of 54.5% compared to 71.7% across England.
Figure 1 - Baby's First Feed 2020/21
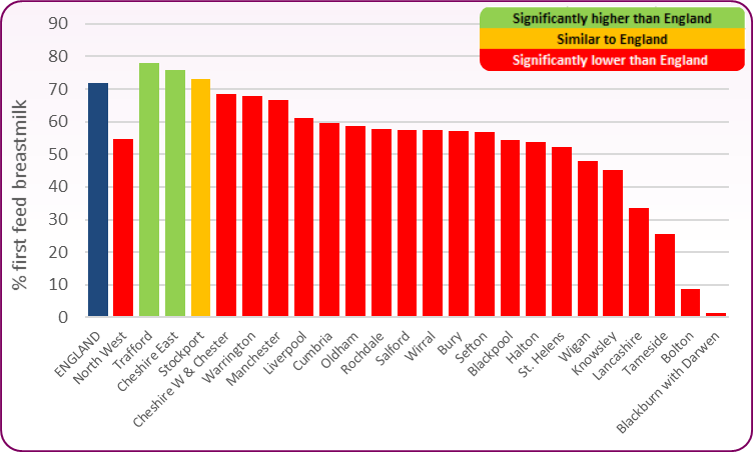 Source: OHID, Child and Maternal Health Profile, Breastfeeding
Source: OHID, Child and Maternal Health Profile, Breastfeeding
Inequalities in baby's first feed, 2020/21
Breastfeeding rates vary across different groups of women; women who are younger, left education earlier, are living in more socially disdavantaged areas, are of White British ethnicity and were born in the UK are the least likely to breastfeed. Figure 2 shows the differences in baby's first feed across England by deprivation, age, ethnicity, complex social factors andd prematurity.
Figure 2: Inequalities in breastfeeding across England, 2020/21
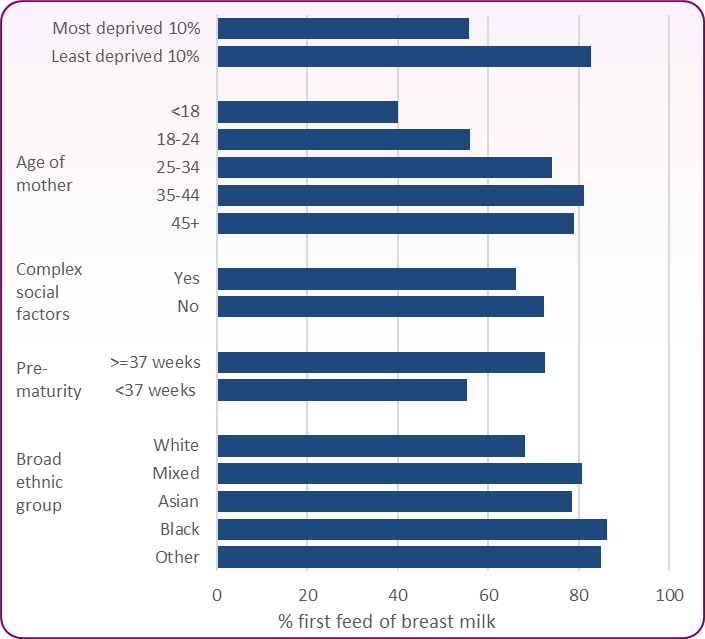 Source: OHID, Child and Maternal Health Profile, Breastfeeding
Source: OHID, Child and Maternal Health Profile, Breastfeeding
Breastfeeding at 6 to 8 weeks
This is the number and proportion of infants that are totally or partially breastfed at 6 to 8 weeks of age. Totally breastfed is defined as infants who are exclusively receiving breast milk at 6-8 weeks of age - that is, they are not receiving formula milk, any other liquids or food. Partially breastfed is defined as infants who are currently receiving breast milk at 6-8 weeks of age and who are also receiving formula milk or other liquids or food.
In 2022/23 in Blackpool, 367 infants were known to be still breastfeeding at 6-8 weeks. This equates to 24.8% of all infants due a 6 to 8 week check, compared to 49.2% in England as a whole3. Due to recording and reporting issues, recent levels of the known breastfeeding status of infants in Blackpool have been lower than the validation threshold for OHID reporting (78.9% in 2022/23 compared to a threshold of 95%). This means that the actual numbers may be higher than reported, though proportions are still likely to be significantly lower than the national average.
Figure 3 compares the rate of breastfeeding at 6-8 weeks after birth in Blackpool with England. Proportions of breastfeeding among all infants due a 6 to 8 week check. While England's trend is gradually increasing, Blackpool has a fairly stable level trend.
Figure 3: Breastfeeding at 6-8 weeks after birth 2015/16 - 2022/23 (all infants due 6-8 week check)
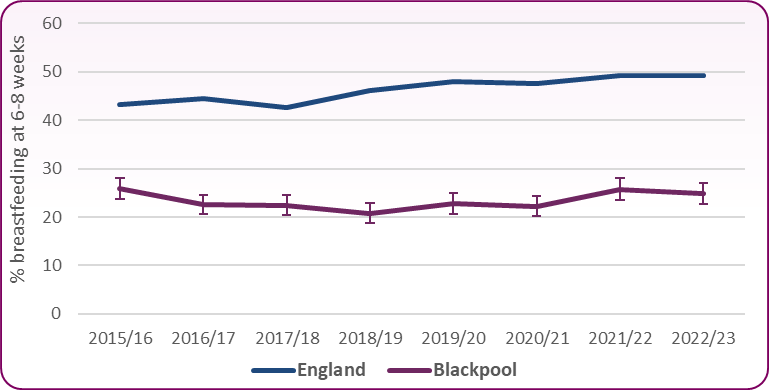 Source: OHID, Breastfeeding prevalence at 6 to 8 weeks after birth
Source: OHID, Breastfeeding prevalence at 6 to 8 weeks after birth
Breastfeeding Drop-Off
The drop off rate is the difference between breastfeeding initiation from birth, and the number of mothers that continue to breastfeed at 6-8 weeks. Approximately a third of Blackpool mothers (32.3%) cease breastfeeding by 6-8 weeks compared to a quarter across England as a whole.
Barriers to Breastfeeding
Public Health England and Unicef UK have developed guidance to support the commissioning of evidence-based interventions to improve breastfeeding rates. The guidance highlights reasons why mothers in England don't breastfeed.
 Source: PHE, Commissioning infant feeding services: infographics, July 2016
Source: PHE, Commissioning infant feeding services: infographics, July 2016
The US Surgeon General's report Call to Action to Support Breastfeeding also identifies a number of barriers to breastfeeding:
- Lack of knowledge
- Social norms
- Poor family and social support
- Embarrassment
- Lactation problems
- Employment and child care
National and local strategies
- The Healthy child programme (Office for Health Improvement and Disparities, 2023) - Aims to increased rates of breastfeeding initiation and continuation, which will contribute specifically to improving breastfeeding and obesity outcomes.
- NICE Guidance [PH11] Maternal and child nutrition (November 2014) covers advice and information regarding breastfeeding.
- The NHS Long Term Plan (January 2019) recommends Unicef UK Baby Friendly accreditation across all maternity services and includes a focus on improved support for families with infants in neonatal care.
-
PHE, Infant feeding: commissioning services. Evidence-based good practice prompts for planning local comprehensive breastfeeding support interventions. Public Health England and Unicef UK have developed the guidance to support the commissioning of interventions to improve breastfeeding rates across England. July 2016
[] NHS, Benefits of breastfeeding [Accessed January 2024]
[] OHID, Small area associations between breastfeeding and obesity, June 2022
[] Data note: These values should be viewed with caution due to data quality issues. High levels of reported 'unknown' breastfeeding status can affect data reliability.