Antenatal and newborn screening
Last Modified 28/03/2023 09:35:10
Share this page
Introduction
Antenatal and newborn screening programmes are an important element of high quality maternity care and are in place to detect a range of conditions, which might increase disability if not identified early in the antenatal or neonatal period.
The antenatal and newborn screening timeline offers a visual reference to optimum times for NHS antenatal and newborn screening tests to take place.
Antenatal screening
The NHS Infectious Diseases in Pregnancy Screening (IDPS) Programme recommends screening to all pregnant women for hepatitis B, HIV and syphilis. Currently, all eligible women in England should be offered screening for infections in pregnancy that can significantly reduce the risk of vertical transmission from mother to child.
-
- HIV weakens the immune system making it difficult to fight off infections. It can eventually lead to AIDS (acquired immune deficiency syndrome). Treatment in pregnancy greatly reduces the risk of passing on HIV to the baby from 1 in 4 (25%) to less than 1 in 200 (0.5%).
- Hepatitis B affects the liver and can cause acute (immediate) and chronic (long-term) ill health. Specialist care is needed for pregnant women with hepatitis B. Vaccination of the baby in the first year of life greatly reduces the risk of the baby developing hepatitis B.
- Syphilis is an infection passed on through sexual contact. It can be passed from mother to baby during pregnancy. If it is untreated, it can result in serious health problems for the baby or cause miscarriage or stillbirth.
The NHS Sickle Cell and Thalassaemia (SCT) screening programme identifies people who are genetic carriers for sickle cell, thalassaemia and other haemoglobin disorders. If 2 people who are carriers have a baby together, there is an increased risk that their baby could inherit a haemoglobin disorder. Screening for SCT is offered to all pregnant women. It is also offered to the baby's biological father if the mother is found to be a carrier of or have a sickle cell or thalassaemia condition1.
The NHS fetal anomaly screening programme (FASP) offers screening for fetal anomalies, Down's, Edwards' and Patau's syndromes. The combined test involves a blood test and an ultrasound scan. All women in England are offered screening for Down's syndrome using this test. Screening for Patau's and Edwards' syndromes using the combined test started in 2015 and is now available across England2.
Newborn screening
The NHS newborn blood spot (NBS) screening programme offers blood spot screening, also known as the heel prick test to find out if a baby has one of nine rare but serious health conditions. Most babies screened won't have any of these conditions but, for the few who do, early treatment can improve their health and prevent severe disability, and even death3.
-
- Sickle cell disease
- Cystic fibrosis
- Congenital hypothyroidism
- 6 inherited metabolic diseases
The NHS newborn hearing screening programme (NHSP) aims to identify moderate, severe and profound deafness and hearing impairment in newborn babies. Early identification of hearing impairment gives children a better chance of developing speech and language skills, and of making the most of social and emotional interaction from an early age
The NHS newborn and infant physical examination (NIPE) includes specific screening tests to find out if your baby has any problems with their eyes, heart, hips and, in boys, the testicles (testes). NIPE screens newborn babies within 72 hours of birth, and then once again between 6 to 8 weeks.
Facts and figures
Data on antenatal screening programmes is at maternity unit level; that is, for all women who attend Blackpool Hospitals, not just for Blackpool residents. NICE guidance4 covers the care that healthy women and their babies should be offered during pregnancy and aims to ensure that pregnant women are offered regular check-ups, information and support. An indicator of care is the proportion of women who receive antenatal assessment before 13 weeks gestation (Figures 1). Figure 2 shows all antenatal assessment by length of gestation.
-
- In 2019/20 2,140 (85.3%%) of women attending Blackpool Teaching Hospital received their antenatal assessment before 13 weeks gestation
- This is higher than the national average of 81.3%
Figure 1: Proportion of women who have an antenatal assessment before 13 weeks gestation, England and Blackpool Teaching Hospital, 2014/15 to 2019/20
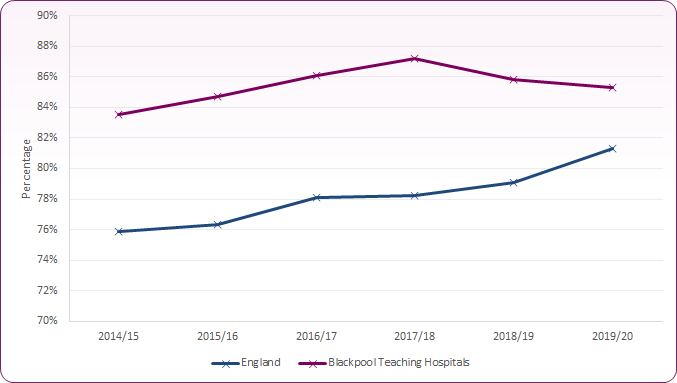 Source: NHS Digital, Hospital Maternity Activity, 2014/15 to 2019/20
Source: NHS Digital, Hospital Maternity Activity, 2014/15 to 2019/20
Figure 2: Antenatal assessment by gestation, England and Blackpool Teaching Hospital, 2019/20
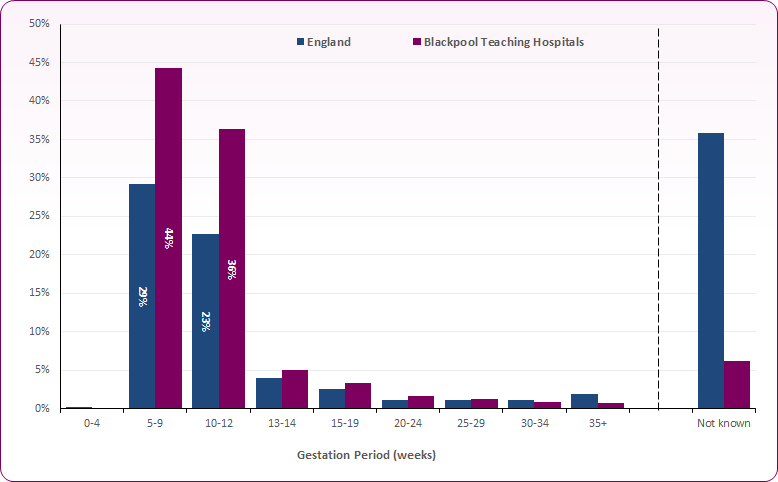 Source: NHS Digital, Hospital Maternity Activity, 2019-20
Source: NHS Digital, Hospital Maternity Activity, 2019-20
Public Health England (PHE) publish data at regional and national level for HIV, sickle cell and thalassaemia, Hepatitis B and Syphilis screening coverage. Figure 3 shows screening uptake for all four conditions is generally lower in the North West than across England, though the difference has been reducing over recent years. Coverage is consistently above the 95% acceptable standard.
Figure 3: Antenatal screening coverage - HIV, Hep B, Syphilis, and Sickle Cell / Thalassaemia: England and the North West
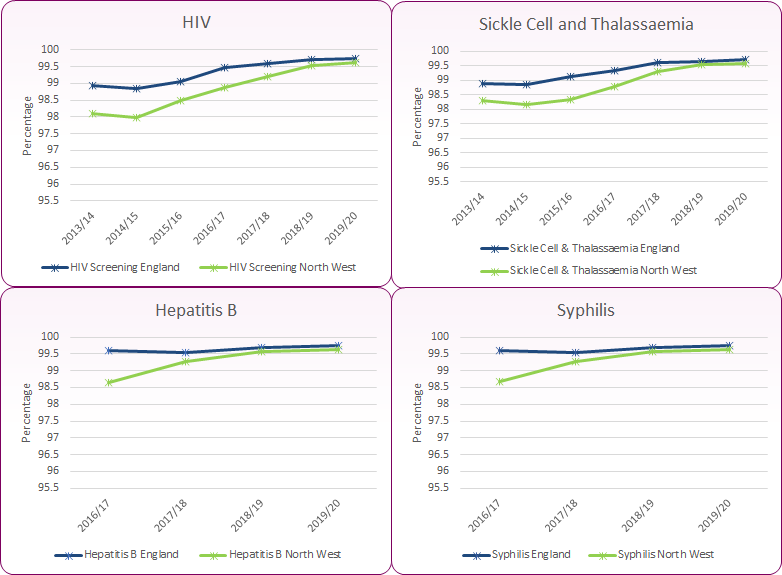 Source: PHE, Public Health Profiles
Source: PHE, Public Health Profiles
Blackpool Teaching Hospitals antenatal screening coverage for HIV infection and sickle cell and thalassaemia is consistently high and above the national target level of 95%. In 2019/20, 99.8% of eligible women were screened for HIV, and for sickle cell and thalassaemia. Fetal anomaly screening (the completion of laboratory request forms) and fetal ultrasound testing levels were also regularly higher than the national average in 2019/20, and well above the 97% national target5.
Newborn Screening
Newborn screening indicators provide an opportunity to track and monitor uptake levels of a variety of screening programmes that have a significant impact on the health and well-being of the population6. Data from NHS screening programme annual reports shows the proportion of babies registered within the Blackpool CCG who have their blood spot result recorded on the child health information system (CHIS) by 17 days of age has been above the 95% target for the last four years (Figure 4).
Figure 4: Trend in coverage of newborn blood spot screening (%), Blackpool CCG, the North Region and England
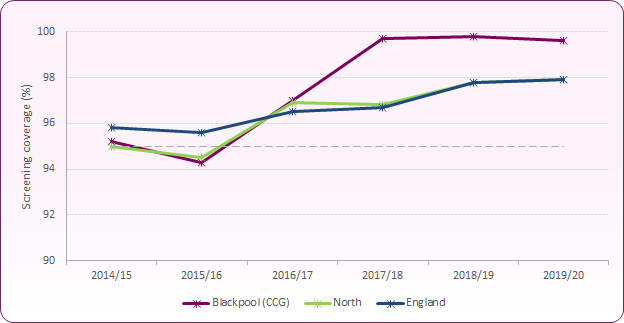 Source: PHE, NHS Screening Programmes, KPI Reports 2014/15 to 2019/20
Source: PHE, NHS Screening Programmes, KPI Reports 2014/15 to 2019/20
Coverage of newborn hearing screening has been consistently above the current 98% target locally and nationally (Figure 5 - 2016/17 data not available).
Figure 5: Trend in coverage of newborn hearing screening (%), Blackpool, the North West and England
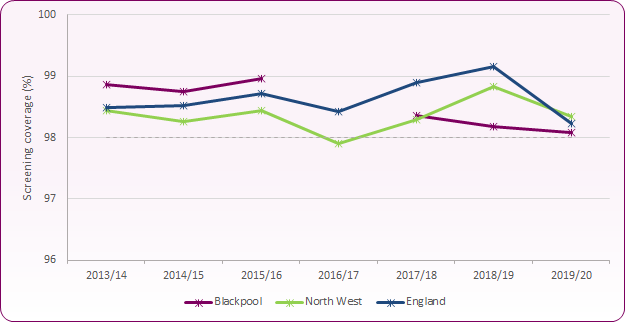 Source: PHE, Public Health Profiles / National Hearing IT Systems
Source: PHE, Public Health Profiles / National Hearing IT Systems
Figure 6 shows the proportion of newborn babies receiving physical examination screening at Blackpool Teaching Hospitals NHS Trust has been higher than the national average and above the 95% target for screening for the last four years.
Figure 6: Newborn physical examination screening - % who are tested for all 4 components (3 components in female infants) within 72 hours of birth
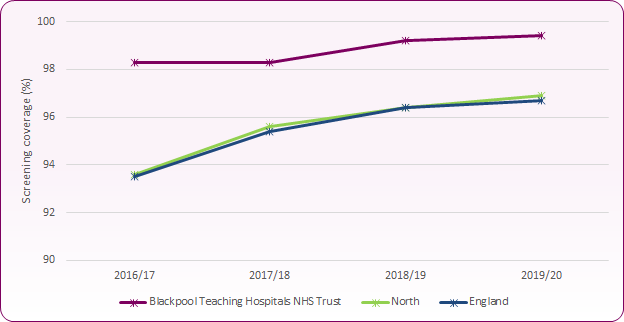 Source: PHE, NHS Screening Programmes: KPI Reports 2016/17 to 2019/20
Source: PHE, NHS Screening Programmes: KPI Reports 2016/17 to 2019/20
Strategies and Guidance
NICE guideline [CG62] Antenatal care for uncomplicated pregnancies (January 2017) covers the care that healthy women and their babies should be offered during pregnancy
NICE quality standard [QS65] Hepatitis B (July 2014) covers testing, diagnosis and management of hepatitis B in children (from birth), young people and adults.
PHE Screening BLOGs provide up to date news from all NHS screening programmes
[] PHE Screening, Sickle cell and thalassaemia screening: fathers matter, March 2017
[] NHS Choices, Screening for Down's, Edwards' and Patau's syndromes
[] NHS Choices, Newborn blood spot test
[] NICE guideline [CG62] Antenatal care for uncomplicated pregnancies (January 2017)
[] Source: NHS screening programmes: KPI reports and briefings 2019 to 2020.
[] Data notes: Different newborn screening indicators are reported at local authority, Clinical Commissioning Group and NHS Trust levels, hence differences in presentation. For newborn screening, 2019/20 data has been affected by Covid-19. Newborn examination screening data should be used with caution due to incomplete data at national level affecting reliability.